This program does not cover out-of-pocket costs for any patient whose commercial insurance plan does not apply Repatha Copay Card payments to satisfy the patients copayment deductible or coinsurance for Repatha. Instead of Medicare Use a Coupon If your Medicare co-pay is higher than 48257 you can save money by using a GoodRx coupon instead.
 Insurance Support And Coverage Repatha Evolocumab
Insurance Support And Coverage Repatha Evolocumab
The cost for Repatha subcutaneous solution 140 mgmL is around 258 for a supply of 1 milliliter s depending on the pharmacy you visit.
Repatha cost with insurance. Most patients do not pay the list price. The cost for Repatha evolocumab subcutaneous solution 140 mgmL is about 25800 for one of the 140 mg single-use prefilled autoinjectors or a prefilled syringe. Call your local insurance commissioner and report it.
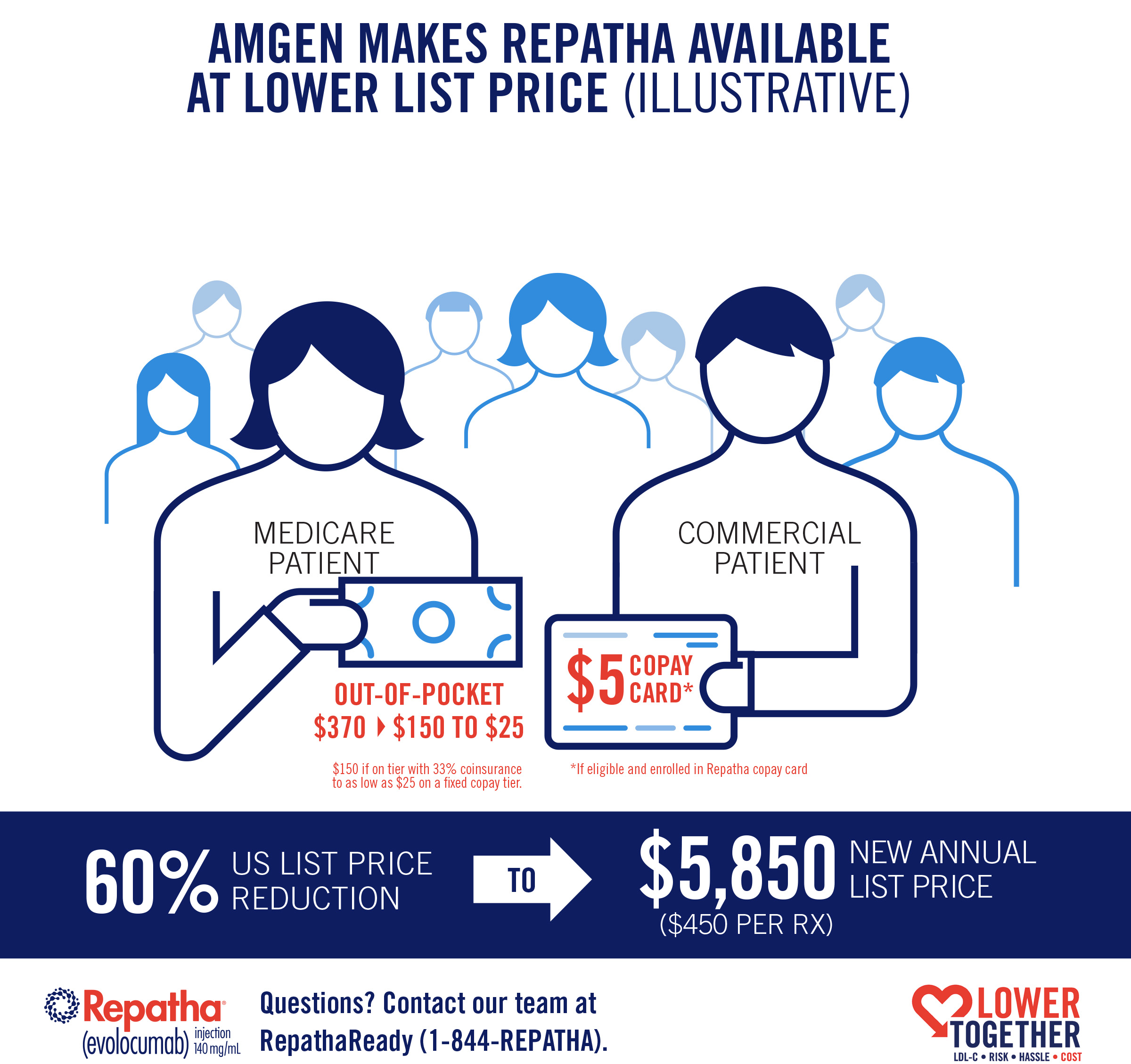
Amgen said Wednesday it is immediately cutting the price of the cholesterol drug Repatha by 60 percent from about 14000 to 5850 per year. Average costs for Repatha with Medicare drug coverage 1. There are some plans associated with CVS that are still covering Repatha so you may not be affected.
The list price for Repatha is 47655 per month. Repatha has not been studied in patients with severe kidney or. If you are covered through a CVS insurance plan you may be asked by CVS to switch from Repatha to another medication.
The 2-pack carton costs roughly 507. Your actual cost will vary and will depend on your insurance coverage. Amgen decided that lowering the list price of Repatha was the best way to help make the drug more affordable to people with Medicare.
Full LIS Medicare patients pay no more than 895 per Repathaprescription. Ways to Save on Repatha Here are some ways that may lower the cost of your Repatha prescription. Currently Amgen estimates that patients on standard Medicare plans pay between 280 to 370 dollars a month out of pocket for their Repatha prescriptions.
As the fastest growing pharmacy program in the country Prescription Hope can obtain Repatha for individuals at the set price of 5000 per month. Usually CVS will send you a letter to notify you. Prices are for cash paying customers only and are not valid with insurance plans.
The cost for Repatha subcutaneous solution 140 mgmL is around 244 for a supply of 1 milliliters depending on the pharmacy you visit. This price is for cash paying customers only is not valid with insurance and may change depending upon the pharmacy. This will however depend on your plans formulary or the list of medications covered by your plan.
With Medicare Part D and most commercial policies covering the drug according to Repatha the average price without any insurance coverage was about 1200 for two prefilled 140MGML syringes. The medication is self-injected and can usually be purchased from a retail pharmacy meaning it falls within the guidelines for Medicare drug coverage. By comparison Repatha which is sold by Amgen has a list price of 14100 a year while Praluent which is marketed by Sanofi and Regeneron costs.
If you have commercial or private insurance you may be eligible to pay no more than 5 for each Repatha prescription with the Repatha Copay Card. For more information regarding Repatha and its effects consult your physician. If patient qualifies the Repatha Copay Card may cover out-of-pocket costs for Repatha up to an annual maximum dollar limit.
Ask your healthcare provider for advice when it comes to purchasing your medications. Note that CVS pharmacies still dispense Repatha. The LIS program also known as Extra Help limits prescription out-of-pocket costs for eligible Medicare Part D patients with limited income and resource limits.
Oct 25 2018 at 850 AM. The majority of commercial and Medicare plans cover Repatha. Prices are for cash paying customers only and are not valid with insurance plans.
Repatha copays have been in the range of 280 to 370 per month for Medicare Part D patients but should drop to 25 to 150 per month after the list price change MedPage Today reported. This program is not open to patients receiving prescription reimbursement under any federal state or government-funded healthcare program. Annual maximum savings amount is 5500.
The 5850 list price should lower monthly costs to around 25 to 150 for Medicare Part D patients according to the drugmaker. 39 Related Question Answers Found Does Repatha affect the liver. If Repatha is administered in.
The cost of Repatha from what we researched seemed to be the same cost at most of the pharmacies we talked with such as Costco Kroger Walmart Sams Club and CVS to name a few. Learn more about LIS or call 1-844-REPATHA. Your copay and deductible costs for any prescription drug can vary depending on what coverage stage youre in.
How much does Repatha cost without insurance. Repatha is covered by most Medicare benefits plans under Medicare Part D the prescription drug benefit. Its not always easy to file a complaint with your states insurance commissioner but there are resources to help you understand the process.