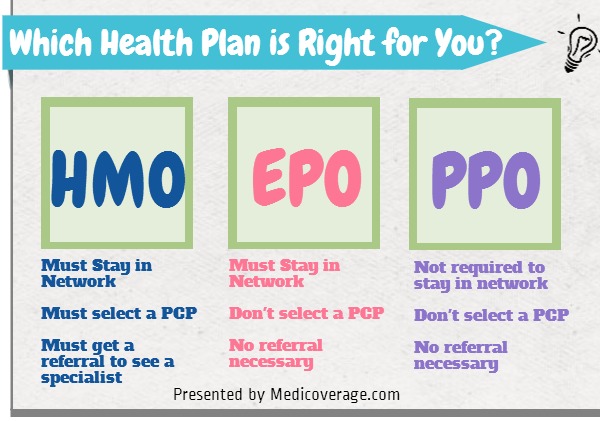
In the US authorization of medical necessity by a primary care physician before a health care service is performed. In medical billing pre authorization is a pre-approval before providing medical service.
 Authorization To Release Healthcare Information
Authorization To Release Healthcare Information
Authorization is a security mechanism to determine access levels or userclient privileges related to system resources including files services computer programs data and application features.

Authorization medical definition. This is the process of granting or denying access to a network resource which allows the user access to various resources based on the users identity. Medical devices are products or equipment intended generally for a medical use and are regulated at Member State level. A HIPAA authorization is a detailed document in which specific uses and disclosures of protected health are explained in full.
By signing the authorization an individual is giving consent to have their health information used or. ˌɔːθ ə raɪˈzeɪʃ ə n us ˌɑːθɚəˈzeɪʃ ə n official permission for something to happen or the act of giving someone official permission to do something. Authorization Health Care Law and Legal Definition An authorization refers to a verbal or written approval from a managed care organization MCO which authorizes the Center for Medicare and Medicaid Services CMS to disclose personal health information to persons or organizations that are designated in the approval.
In pharmacy a cost-containment procedure that requires a prescriber to obtain permission to prescibe a medication prior to prescribing it. Medical records cannot be disclosed without authorization from the patient. How to use pre-authorization in a sentence.
During their review the insurance company may decide a generic or another lower cost alternative may work equally well in. A referring health care provider must be able to document why the procedure is needed. Will the HIPAA Privacy Rule hinder medical research by making doctors and others less willing andor able to share with researchers information about individual patients.
Shiel Jr MD FACP FACR Prior authorization. Sometimes called prior authorization prior approval or precertification. Medical Dictionary for the Dental Professions Farlex 2012.
Learn about prior authorization by reviewing the definition in the HealthCaregov Glossary. Synonyms Antonyms Example Sentences Learn More about authorization. The act of authorizing.
Authorization is getting approval from the insurer before a procedure. A confirmation of a users access level within a network after successful log-in and authentication. Marketing authorisation is the process of reviewing and assessing the evidence to support a medicinal product such as a drug in relation to its marketing finalised by granting of a.
An insurance plan requirement in which the service provider must notify the insurance company in advance about certain medical procedures or services in order for coverage to be considered. For example some brand name medications are very costly. Formal approval by the gatekeeping arm of a third-party payer for payment of a requested procedure.
It still does not guarantee coverage. 2012 Farlex Inc. A decision by your health insurer or plan that a health care service treatment plan prescription drug or durable medical equipment is medically necessary.
Authorization as by an insurer that is required prior to performance of a health-care service such as a surgery or prescription of a drug. The Medical Devices and the In-Vitro Diagnostic Devices Regulations have introduced new responsibilities for the European Medicines Agency EMA and national competent authorities in the assessment of certain categories of medical device. The prior authorization process gives your health insurance company a chance to review how necessary a certain medication may be in treating your medical condition.
Medical Definition of Prior authorization Medical Author. An instrument that authorizes. Pre-authorization definition is - prior authorization.