Box Office Mojo Find Movie Box Office Data. The HealthMarkets Customer Service team is your ally.
 Create A Health Insurance Marketplace Account Healthcare Gov
Create A Health Insurance Marketplace Account Healthcare Gov
711 WellFirst Employee Health Plan 877-274-4693 TTY.
Health marketplace customer service phone number. This is Healthcare Marketplace. 7500 Security Boulevard Baltimore MD 21244. Individual Marketplace Plans 866-514-4194 TTY.
Customer Service Were with you every step of the way. To 8 pm Monday through Friday. For more information about HealthMarkets Insurance Agency send us an email or call one of the numbers provided to speak with an agent.
1-855-889-4325 When open enrollment starts on October 1 2013 youll be able to. Amazon Web Services Scalable Cloud Computing Services. Behavioral HealthSubstance Abuse Benefits.
South Dakota Health Insurance Marketplace 800-318-2596. For Sparrow Health System inquiries please call 5173648432 or toll free 8772750076. We know youve got questions about the new Health Insurance Marketplace.
Appeals 465 Industrial Blvd London KY 40750-0061. Book Depository Books With Free Delivery Worldwide. Answering your questions is.
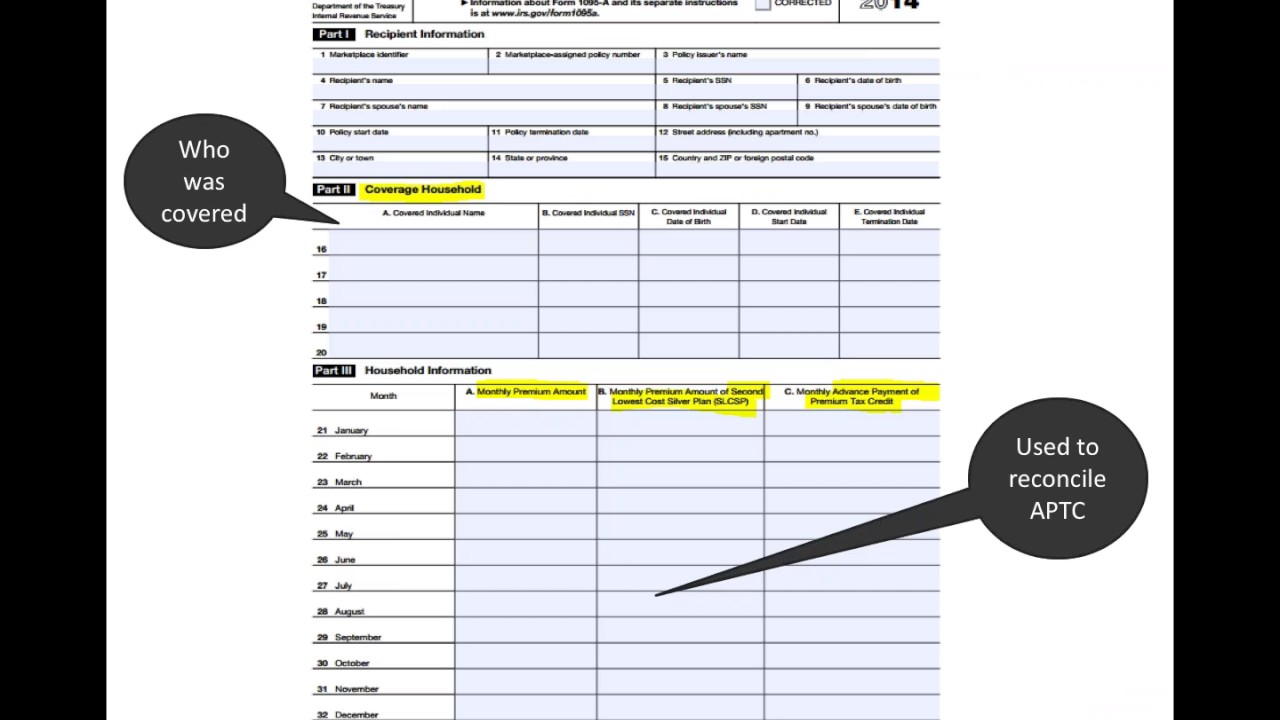
Centers for Medicare Medicaid Services. Whether youre celebrating a new baby home job or relationship well make sure youre covered. Information about changes to your address income or household size unless the Marketplace has asked for it.
Sign in to your Medicare Advantage member site. Original documents of any type. A federal government website managed and paid for by the US.
Call us at 1-800-318-2596. Health Insurance Marketplace is a registered trademark of the Department of Health and Human Services. For Marketplace inquiries please call 5173648567 or toll free 8665393342.
For Hoosier Healthwise and Healthy Indiana Plan MDwise customer service is available at 1-800-356-1204. In case of emergency call 9. Centers for Medicare Medicaid Services.
24 hours a day 7 days a week. DO NOT SEND the following kinds of documents in the mail. Our knowledgeable representatives are ready to help you.
Home Services Experienced Pros Happiness Guarantee. Weve received thousands of them over the past month. Federal Relay Services TTY Access for Deaf Hard of Hearing.
This page is out-of-date Get the latest information here. 1-800-ASK-USPS 1-800-275-8777 Hours of Operation Monday Friday 8 AM 830 PM ET Saturday 8 AM 6 PM ET. Help is available from 8 am.
Help is available from 8 am. 1-800-721-0627 TTY 711 for technical issues 700 AM to 1000 PM CT 7 days a week. Healthcare Marketplace Healthcaregovs Best Toll-Free800 Customer Phone Number.
To 8 pm Monday through Friday. Identify Whether an Email Phone Call Text Message or Webpage is from Amazon Request the Closure of Your Account and the Deletion of Your Personal Information More in Security Privacy. Connect with our customer service representatives to help resolve your issue and get back on track.
Health Insurance Marketplace Attn. Effective September 1 2019. Audible Listen to Books Original Audio Performances.
A new 800 number you can call to get your Marketplace questions answered by a customer service representative available 247. Call the number on your member ID card for general health plan information. Amazon Ignite Sell your original Digital Educational Resources.
7500 Security Boulevard Baltimore MD 21244. You can contact WellFirst Health Customer Care at the following numbers. Sign in to your Medicare Prescription Drug Plan member site.
Contact Meritain Health customer service. Contact HealthMarkets - HealthMarkets. USPS Customer Service Call.
South Carolina Health Insurance Marketplace 800-318-2596. Tennessee Health Insurance Marketplace 800-318-2596. ComiXology Thousands of Digital.
We can help you with. Healthcare Marketplace Healthcaregov Phone Number Calling Healthcare Marketplace Healthcaregov customer service faster by GetHuman. A federal government website managed and paid for by the US.
Health Insurance Marketplace is a registered trademark of the Department of Health and Human Services. For PPOInsurance Company inquiries please call 5173648456 or toll free 8002039519.