Medicare will only cover your DME if your doctors and DME suppliers are enrolled in Medicare. Medical supplies that may be needed for patients to care for themselves at home eg ostomy supplies are a separate issue from supplies needed to maintain durable medical equipment.
Https Www Kmap State Ks Us Documents Content Bulletins 12031b 20 20dme 20 20per 20diem Pdf
1 2 Nondurable medical equipment devices and supplies are manufactured for one-time use only and are disposable.
Are ostomy supplies considered dme. Medical supplies that are used with covered DME are covered when the supply is necessary for the effective use of the itemdevice eg oxygen tubing or mask or tubing for a delivery pump. Generally Medicare Part B covers 80 percent of allowable charges for ostomy supplies. Ostomy Supplies Ostomy Supplies are limited to the following.
D urable medical equipment devices and supplies are reusable products used for the treatment of an illness or injury that are typically ordered by a physician or other health care provider for use in a patients place of residence. Doctors and suppliers have to meet strict standards to enroll and stay enrolled in Medicare. Durable Medical Equipment DME and Medical Supply Services Provider Fee Schedule for All Medicaid Recipients.
If beneficiary is in a covered 60-day home health care episode ostomy supplies are not billable to DME MAC. If it is used once and then thrown away it is considered a durable medical supply. Insulin pumps are considered DME.
Some durable medical equipment prosthetics orthotics and medical supplies. Pouches face plates and belts Irrigation sleeves bags and ostomy irrigation catheters Skin barriers Benefits are not available for deodorants filters lubricants tape appliance cleaners adhesive. Some durable medical equipment.
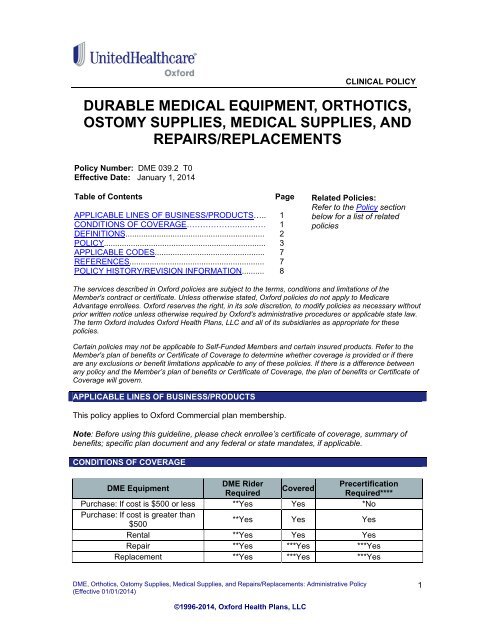
Durable Medical Equipment Orthotics Ostomy Supplies Medical Supplies and RepairsReplacements Page 4 of 7 Depending on individual circumstances people who pay out-of-pocket for. Durable medical equipment DME is equipment that can withstand repeated use. Rehabilitative and assistive technology items are considered non-standard or specialty items and are generally obtained.
Ostomy supplies ordered for a member during an authorized home health care plan is restricted to equipment that. Supplies can also include bandages catheter equipment needles for injection kits and diapers. Ostomy supplies fall into a category known as prosthetic devices and Medicare coverage of durable medical equipment prosthetics orthotics and supplies DMEPOS applies.
Supplies must be provided by home health agency with payment included in home health prospective payment system PPS. Medical Supplies that are used with covered DME are covered when the supply is necessary for the effective use of the itemdevice eg oxygen tubing or mask batteries for power wheelchairs and prosthetics or tubing for a delivery. These types of medical supplies are not address in this guideline.
Durable Medical Equipment Orthotics Ostomy Supplies Medical Supplies and RepairsReplacements Medicare Advantage Coverage Summary Durable Medical Equipment DME Prosthetics Corrective AppliancesOrthotics Non-Foot Orthotics and Medical Supplies. The maximum fee for ostomy supplies is per stoma or per fistula unless otherwise. 000 the procedure code is considered non-classified and the provider must request prior authorization or submit a By Report claim.
Medical Supplies that are used with covered DME are covered when the supply is necessary for the effective use of the itemdevice eg oxygen tubing or mask batteries for power wheecl hairs and prosthetci s or tubing for a delivery pump. Ostomy Supplies are limited to the followni g. Medicare Part B Medical Insurance covers Medically necessary ostomy supplies if youve had a colostomy ileostomy or urinary ostomy.
Durable medical equipment is prescribed for long-term use to help those in recovery from an illness or injury. Careful research by the consumer is necessary in these situations because although having the insurer pay for some of the cost may seem like the best deal it may not be. Your costs in Original Medicare.
Make sure your doctors and DME suppliers are enrolled in Medicare. Medicare covers the amount of supplies your doctor says you need based on your condition. Ostomy Supplies are limited to the following.
O Irrigation sleeves bags and ostomy irrigation catheters. If your doctors or suppliers arent enrolled Medicare wont pay the claims submitted by them. Now with the insurance I cant get a straight answer whether ostomy supplies fall in the category of Durable Medical Equipment DME which gives examples of wheelchairs walkers crutches and oxygen tanks or non-durable such as disposable dressing and bandagesTheir health bulletin state that medicare considers ostomy supplies to be prosthetic and classifies the supplies as DME but it doesnt state how they consider ostomy supplies.
Orthotic braces that stabilize an injured body part and braces to treat curvature of the spine are considered Durable Medical Equipment. Medical Supplies that are used with covered DME are covered when the supply is necessary for the effective use of the itemdevice eg oxygen tubing or mask batteries for power wheelchairs and prosthetics or tubing for a delivery pump. Although convenience items may be associated with secondary medical uses the principal or primary.
Disease-specific or medically necessary supplies such as ostomy bags and parenteral and enteral nutrition are at least partially covered by some private insurers.
