For HSA-Qualified plans prescription drugs are subject to medical deductible in all three options. You can login to your member account to find in-network pharmacies in your plans network and to compare costs.
 Pharmacy Priority Partners Mco
Pharmacy Priority Partners Mco
If your drug suddenly goes up in price or is no longer covered check to see whether.

What pharmacy takes my insurance. Pharmacy benefits and services from Aetna can help individuals and families make the best choices for their health and budget. That take your plan. Certified Pharmacies You must fill all prescriptions at certified pharmacies in the Philippines.
Pharmacy coverage you will not be able to use Meds by Mail MbM pharmacy benefits. The BlueMedicare Pharmacy Network includes both preferred and standard choices. Your choice of pharmacies will depend on which pharmacies are in your health plans network what kind of medication you need and the quantity.
Find a provider or pharmacy online here. Retail Pharmacy for up to a 30-day supply. Kaiser Permanente Pharmacies Option 1 MedImpact Network-Community Pharmacies Option 2 or Out-of-Network Pharmacies Option 3.
If you dont use a participating network pharmacy you may have to pay the full retail price for your prescriptions. Though we generally accept these providers please contact your insurance provider before your visit to make sure youre covered. At Giant Eagle Specialty Pharmacy our guiding philosophy is to serve as an extension of your practice providing you with a single point of contact for specialty medication access and coordination of insurance benefits and financial assistance.
Associates enrolled in HMOs receive pharmacy benefits through their HMOs. International SOS strives to update the certified pharmacy list on the 1st and 15th of each month. Your preferred pharmacy network includes the.
My CareSource Account. You can get prescriptions filled at Level 1 pharmacies for the same copay or percentage of the drug costs you usually pay as part of your prescription drug plan. On our website scroll down and select Find a Pharmacy.
For an extra copay or percentage of the drug cost depending on your benefit you have more choices with Level 2 pharmacies no matter which drug you fill. Download a copy here. You can choose any pharmacy option regardless of your Flexible Choice provider option.
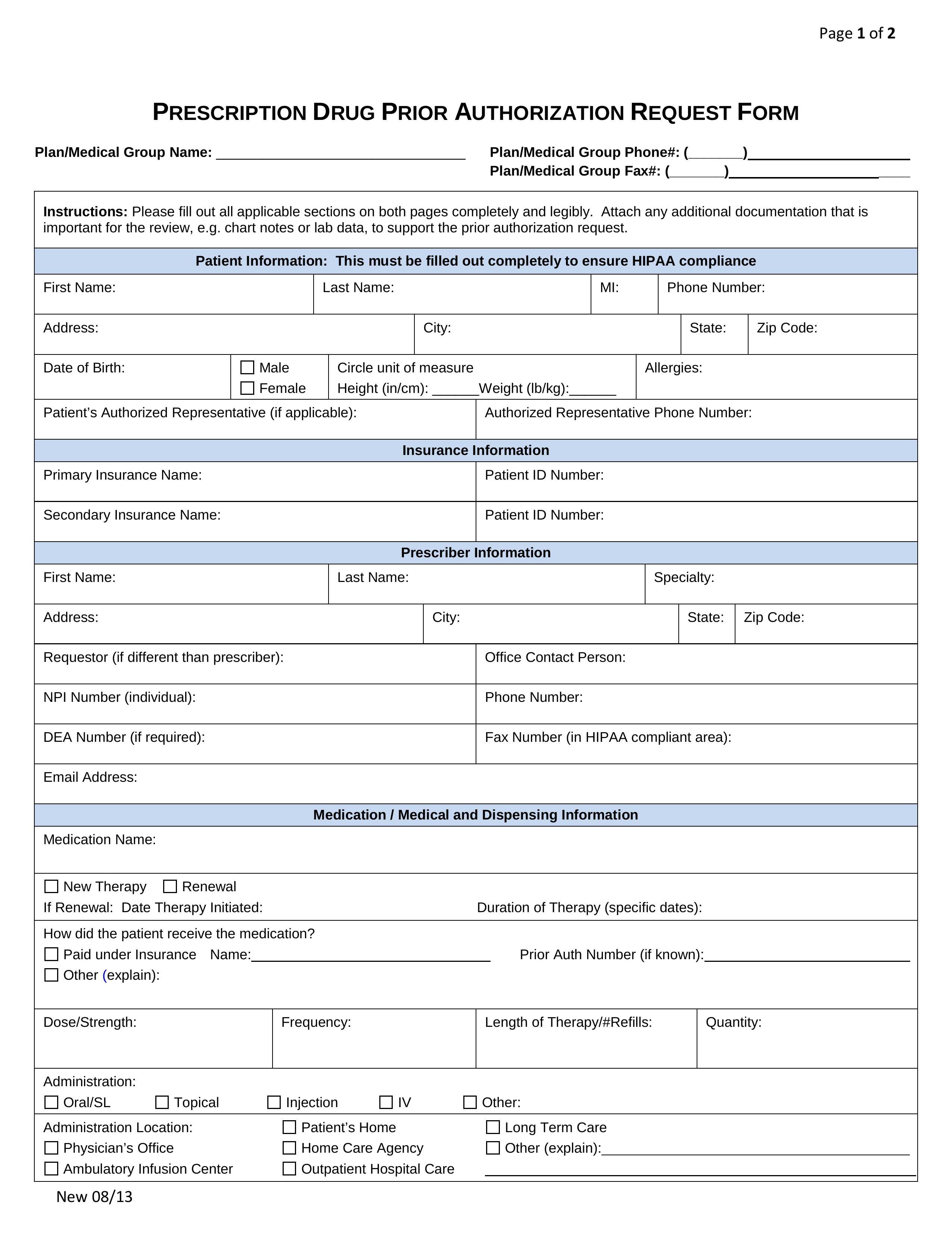
What is the impact on my Meds by Mail MbM pharmacy benefits if I have other health insurance. Additionally most insurance companies also have portals and mobile apps that help you price a drug based on your current insurance plan coverage benefits. The Provider Pharmacy Directory outlines your plans network of Primary Care Physicians Specialists Hospitals Skilled Nursing Facilities Outpatient Facilities Pharmacies and Supplemental Provider contacts.
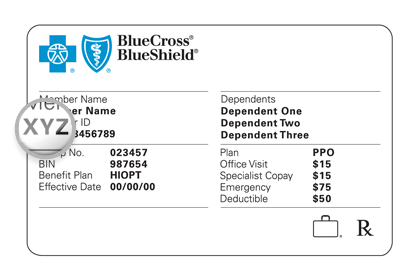
Use the portal to pay your premium check your deductible change your doctor request an ID Card and more. Pharmacies that are a part of the OptumRx network will send the claim electronically to VHA Office of Community Care for payment. Spina Bifida and CWVV beneficiaries can use a local pharmacy in the OptumRx network and the Meds by Mail program to obtain their medications without a cost sharecopay.
Getting your prescriptions filled is as easy as looking up a participating pharmacy near you and presenting your EmblemHealth ID card. Learn more about the coverage and benefits offered by Aetnas pharmacy plans including prescription drug home delivery and condition support programs. If the 1st or 15th falls on a federal holiday or weekend the list will not be updated until the next business day.
If you have any other health insurance OHI that includes. You dont need to enroll for it separately. Your pharmacy options may include.
Choosing a network pharmacy may help you save on costs. You can view list of pharmacies for your plan by signing in to your health plan account. When you fill a prescription at a preferred pharmacy your cost-sharing may be lower than at a standard network pharmacy.
Plans with Your Doctor directory is a summary for informational purposes only. Cigna does not cover annual physicals wellness exams or select lab tests. Search the Certified Pharmacy List.
Start by going to the prescription section under My Coverage. Find a network pharmacy. You have three pharmacy options.
Please notify the VHA Office of Community Care VHA OCC of any changes in your health insurance coverage. On the app go to Express Scripts open the main menu and select Find a Pharmacy. About a quarter of plans require consumers to fill certain prescriptions through mail-order pharmacies.
There youll see only pharmacies in Michigan and the US. Please call Walmart Care Clinic support at 1-844-398-1398 or your insurance. We accept no responsibility or liability for any damages arising from your use of this information.
BlueMedicare members may go to either type of network pharmacy to receive covered prescription drugs. Our Individual Qualified Health Plans Essential Plans and Small Group Plans no longer offer CVS and Target as in-network pharmacy locations. If youre already at the pharmacy you can also ask the pharmacist whether the prescription youre picking up is covered by your insurance.
This listing of providers does not constitute a recommendation of any physician provider group hospitalfacility or other provider. The pharmacy benefit is automatically included in the Premier Saver Contribution eComm PPO and Local Plans.