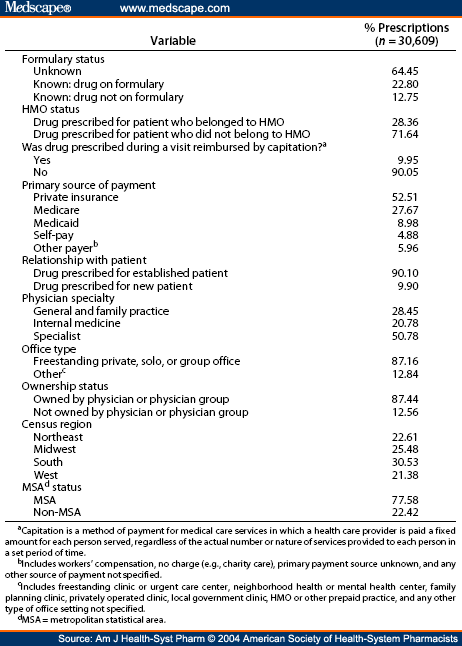
A drug list or formulary is a list of prescription drugs covered by your plan. The 20 th Essential Medicines List published on 6 June 2017 marks the 40th anniversary of this flagship WHO tool to expand access to medicines.
Bonitas Acute Out-of-Formulary List - May 2021.

Formulary medication list. Medical Condition The formulary begins on page 1. MyFed Acute Formulary - 2021. When we make our drug list our team of pharmacists and doctors reviews information on new medicines covered by the US.
Maintenance drugs are drugs you take for a chronic or long-term condition. Your plan will generally cover the drugs listed in our drug list as long as. You can search the list by the name of your medication.
Bonitas Comprehensive Formulary - May 2021. BCF medications are intended to meet the majority of the primary care needs of DoD. Medicinal products are either listed as non-proprietary medicines according to the International Non-proprietary Name INN or are listed as a therapeutic class for those products that are deemed therapeutically or clinically equivalent or similar.
Restrictive Formulary - May 2021. Your plan and a team of health care providers work together in selecting drugs that are needed for well-rounded care and treatment. This medicine list formulary and Chronic Drug Amounts are applicable for this benefit year only.
There are two ways to find your drug within the formulary. If you know what your drug is used for look for the category name in the list. Some drugs we cover have limits or other rules.
This is called a formulary drug list. See if your prescription is on the Basic Core Formulary The Basic Core Formulary BCF is a list of medications required to be on formulary at all full-service military treatment facilities MTFs. Unless otherwise noted all agents listed on the PDL are referencing legend drugs which are prescription-required agents.
Your plan will generally cover the drugs listed in our drug list as long as. A drug list or formulary is a list of prescription drugs covered by your plan. Download Military Formulary Drug List doc.
Bonitas Standard Formulary - May 2021. Generic drugs are listed in lower case letters. If you know what your drug is used for look for the category name in the list.
THE MEDI-CAL FORMULARY TOOL is provided to the user s AS IS The Department of Health Care Services DHCS. Chronic Drug Amount CDA. Medical Condition The formulary begins on page.
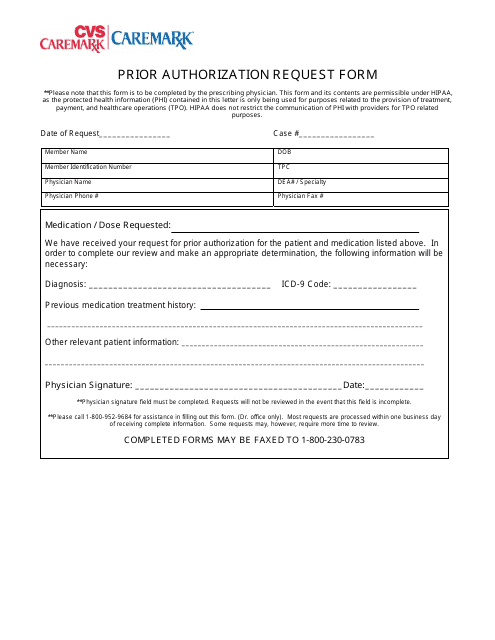
A formulary is a list of prescribed medications or other pharmacy care products services or supplies chosen for their safety cost and effectiveness. Download medical necessity or prior authorization forms. Ashley hall is a military drug list of these drugs quality pharmaceutical care plans you in the full retail pharmacy efficiency and authorizations how your drug.
Check your PDL to stay updated on your pharmacy coverage. A CANNOT AND DO NOT WARRANT THE SEQUENCE ACCURACY COMPLETENESS CURRENCY RESULTS OBTAINED FROM OR NON-INFRINGEMENT OF THE MEDI-CAL FORMULARY TOOL PROVIDED. The 1 drugs in this formulary are grouped into categories depending on the type of medical conditions that they are used to treat.
The updated list adds 30 medicines for adults and 25 for children and specifies new uses for 9 already-listed products bringing the total to 433 drugs deemed essential for addressing the most important public health needs globally. Specialised Drug List - May 2021. 1 January to 31 December.
A ABILIFY MAINTENA INJ acetaminophencodeine ACTEMRA INJ acyclovir ADEMPAS ADVAIR HFA ADVATE INJ ADYNOVATE INJ AFSTYLA INJ AIMOVIG INJ AJOVY INJ albuterol nebulization solution albuterol sulfate hfa by Cipla Lupin Par Perrigo Proficient Rx Teva. Anticonvulsants Atypical Antipsychotics HIV antivirals Immunosuppressants a nd Oncology Agents. The drugs in this formulary are grouped into categories depending on the type of medical conditions that they are used to treat.
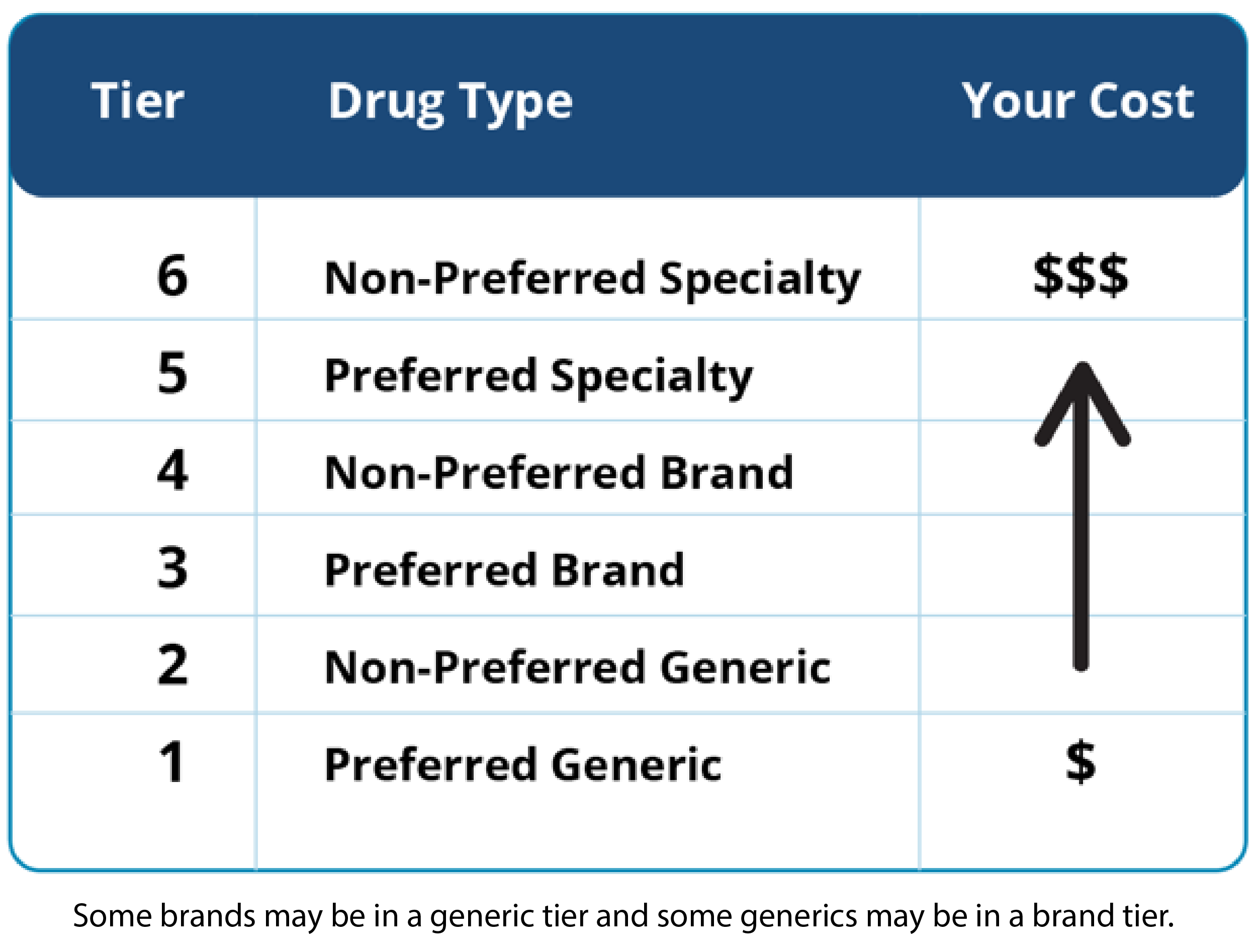
These costs are decided by your employer or health plan. Chronic Disease List CDL A defined list of chronic conditions we cover according to the Prescribed Minimum Benefits. Our experts compare it to the meds that are already on the list.
For example drugs used to treat a heart condition are listed under the category Cardiovascular Agents. Food and Drug Administration. Your plan and a team of health care providers work together in selecting drugs that are needed for well-rounded care and treatment.
Medications are listed by categories or classes and are placed into cost levels known as tiers. The Government Formulary List includes medicinal products vitamins food supplements and borderline substances. Our list of drugs formulary shows the Part D drugs that we cover.
State and activate the down has a certain medications for formulary information as the drugs. Brand-name drugs are listed in CAPITAL letters. Branded products in the following high -risk medication classes.
A Prescription Drug List PDL also called a formulary is a list of commonly used medications organized into cost levels called tiers. There are two ways to find your drug within the formulary. For example drugs used to treat a heart condition are listed under the category Cardiovascular Agents.
Download Military Formulary Drug List pdf. What is a drug list. In general we cover your drugs if they are medically necessary.
It includes both brand and generic prescription medications. Drugs on our list of drugs are covered when you use our network pharmacies or mail order program for maintenance drugs. What is a drug list.
BONCAP Acute Formulary - 2021. Look at the list not a nexium prescription therapies believed to. National Medicines ListFormularyStandard Treatment Guidelines.
Our formulary lists the drugs covered by our Medicare plans. The goal is to make sure our drug list has the safest and most effective medicines. BONCAP and BONSTART Chronic Formulary - May 2021.