So youll need to check your plan details to find out how much youll need to pay out of pocket. Just verify that the plan has coverage for braces without an age limit.
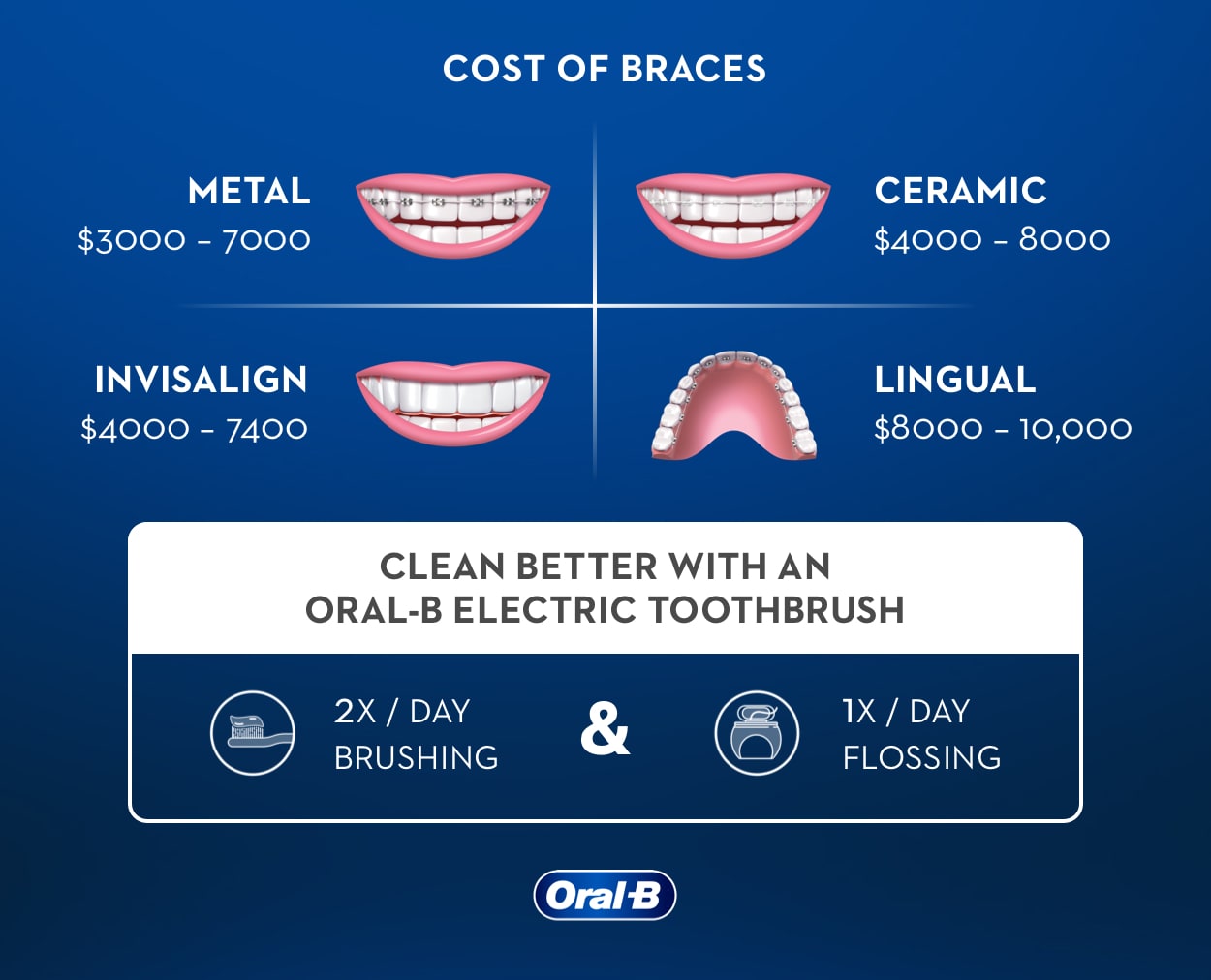 How Much Do Braces Cost Oral B
How Much Do Braces Cost Oral B
Dental insurance typically includes braces for people under 18.

Does ppo insurance cover braces. Many plans whether DeltaCare USA or Delta PPO will provide some sort of coverage for braces. Many of Guardians basic dental HMO or PPO plans will not cover orthodontic treatment while a decent number of their full coverage plans will and that includes Invisalign. If approved the insurance company covers 100 after a yearly deductible for the patient.
Please refer to your Group Dental Service Contract Evidence or Certificate of Coverage or Summary Plan Description for your plans specific coverage limitations and exclusions. Some states require all dental insurers licensed in the state to provide coverage for childrens braces. Brackets can be clear or.
But even if your plan provides orthodontic benefits youll need to carefully review the details because it might have an age limit up to age 19 a lifetime coverage. In most cases it is 350 per year. Ceramic braces These appliances work just like traditional braces except the brackets used are ceramic.
Some plans cover more for children than adults and others have a lifetime limit although they vary based on the specific plan. Dental plans typically dont cover cosmetic procedures such as whitening and veneers but if your child has a medical need for braces difficulty chewing or jaw misalignment your plan may provide coverage. But many of these policies have a cap limit on maximum yearly benefits.
The brackets are then accompanied by light wires that attach to the brackets with tiny rubber bands. Dental insurance typically does not cover orthodontic work for adults but some dental plans do offer some benefits. First off since major medical insurance does not include coverage for dental services in most instances it also generally does not cover braces or other orthodontic services.
Does insurance cover braces in this case. The medically necessary insurance only covers braces with approval from a consulting orthodontist from their insurance company. If you have health insurance for your family the first step is to determine if it includes coverage for braces.
This means you are responsible for dental costs including braces that go. But not all dental plans include orthodontic treatment and if they do it is often limited to children under the age of 18. Dont be surprised to discover that your dental insurance however exemplary it may be does not cover bracesBraces are a major expenditure that can cost you up to 4000 and in extreme cases even more.
Yes as long as you sign up for the right plan. Beware that some insurance plans will only cover braces if theyre deemed medically necessary such as if your child has trouble chewing. Dental insurance is often a part of an employees health care package allowing your employer to decide on the plan and level of coverage.
Many companies offer stand-alone dental policies. You can find plans that cover orthodontic treatments for adults. Dental insurance for braces If you think that braces are in your future either for yourself your spouse or your children you may be interested in having dental insurance that includes orthodontia.
How much do braces cost for kids. Before we answer the question the first thing you should know is whether your PPO or HMO dental plan covers orthodontics or braces. Your policy can contribute at least part.
Traditional braces These devices consist of stainless steel brackets that attach to the front of the teeth. To receive insurance coverage on braces you may need to seek supplementary orthodontic coverage. This means you wont receive insurance payments toward braces or similar treatment regardless of your deductible or annual maximumall.
Payments for orthodontic coverage are specifically excluded. Most dental insurance plans will. All dental plans have an annual cap on services for the year.
Instead youll likely need to look to dental insurance. Things to know about insurance and braces. Your dental insurance will adhere to a more lenient standard of medical necessity provided it includes orthodontia benefits as many do notPlans designed to cover braces may approve your claims after the provider submits evidence of a severe handicapping malocclusion.
Standard dental insurance plans usually dont cover orthodontics and if they do you have to know how long the waiting period is. Today however employers may opt for plans that cover orthodontic treatment for. These answers are only a summary of how most Delta Dental PPO and Delta Dental Premier orthodontic coverage works.
If your employer-sponsored dental insurance plan does not cover braces for adults you can enroll in an individual dental insurance plan. Here are a few things to keep in mind when it comes to getting insurance to pay for treatments with your orthodontist.









/invisalign-and-dental-insurance-coverage-7565b48f924b43c7b9f7f7431be4dcbe.png)
/invisalign-and-dental-insurance-coverage-7565b48f924b43c7b9f7f7431be4dcbe.png)