What they are why you need them. For Commercial Insurance networks this process involves two steps 1 Credentialing and 2 Contracting.
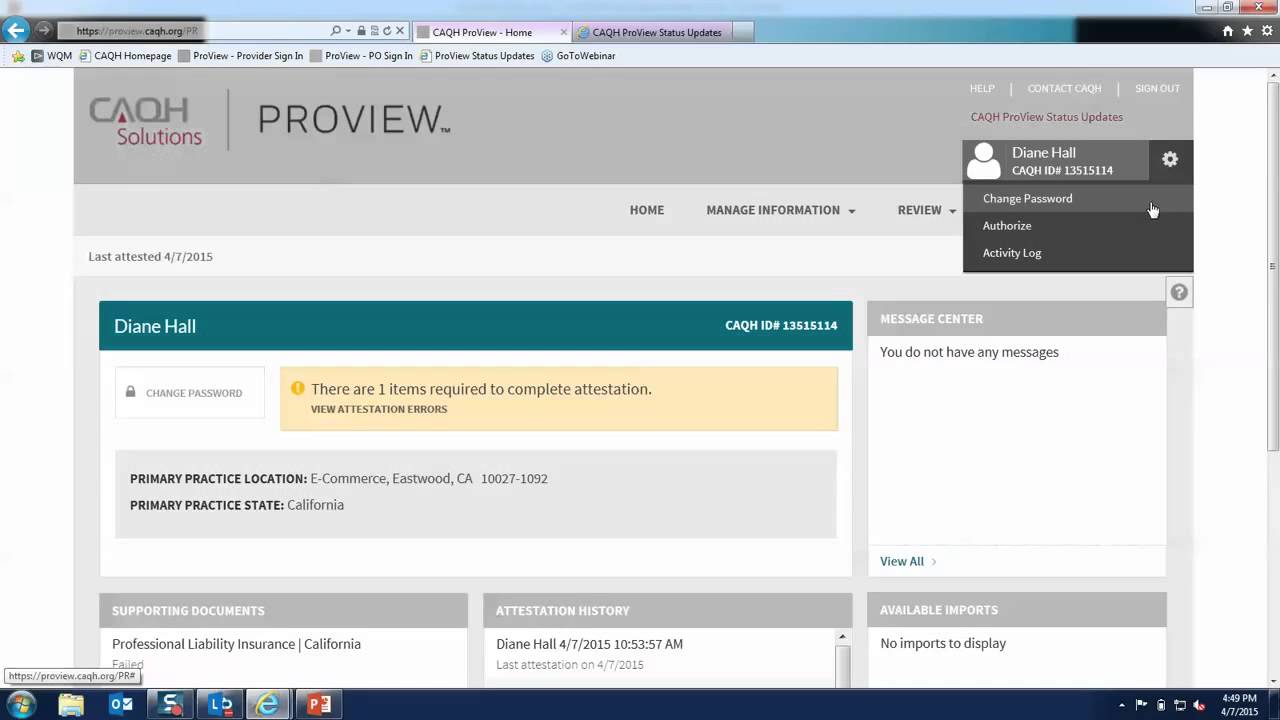 Caqh Proview Provider Portal Overview Youtube
Caqh Proview Provider Portal Overview Youtube
Final discounted rate will be reflected once all.
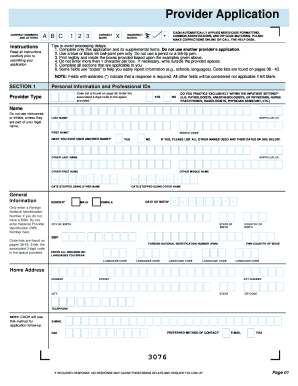
Caqh provider enrollment. CAQH Credentialing refers to the process of practitioners self reporting demographic education and training work history malpractice history and other relevant credentialing information to create an. Welcome to CAQH ProView. Join Josh Plummer and Michelle Pivelja of PractiveWorx for a discussion on the fundamentals of I A NPPES PECOS and CAQH.
Through an intuitive profile-based design you can easily enter and maintain your information for submission to your selected organizations. EnrollHub then sends their enrollment information directly to. CAQH ProView Reference Material.
Provider outside of the system user when EFT processing is complete if additional communication is needed. The real-time provider information in CAQH ProView includes validated key data elements such as TIN NPI DEA and addresses. Change Enrollment Request Pending.
49400 51400 39520 41120. The CAQH CORE Benefit Enrollment Operating Rules support consistent infrastructure and a. The first step is for the provider to submit a participation request to the health plan using their application process.
In addition CAQH will comply with any applicable laws and regulations pertaining to confidentiality and security in the development of the database and the data collection process. SSN number must be 10 characters no all same numbers 9999999999 or sequence numbers 123456789. A CAQH solution EnrollHub combines enrollment capabilities for EFT and Electronic Remittance Advice ERA enabling healthcare providers to use a single secure on-line process to enroll with multiple health plans at once.
This screen is only for self registering providers. I forgot my usernamepassword. Explore CAQH Solutions for provider credentialing and verification directory maintenance coordination of benefits and more.
CAQH is an online data repository of credentialing data. What is CAQH. Please select a format for each part of this series below.
The CAQH database is housed in a. The Benefit Enrollment transaction 834 is used by employers as well as unions government agencies or insurance agencies to enroll members in a healthcare benefit plan. Editing SSN and DOB Quick Reference Guide.
When receiving a provider enrollment request health plans use the credentialing process to ensure that the provider is. Enrolling all but the largest healthcare provider groups in EFT and ERA is often too difficult for health plans. In the past every insurance company had a unique provider enrollment process meaning application forms and credentialing requirements varied from payer to payer.
CAQH is a non-profit alliance of health plans and related associations working together to streamline the business of healthcare. Explore CAQH Solutions for provider credentialing directory maintenance coordination of benefits and more. The Council for Affordable Quality Health Care or CAQH is a nonprofit organization that presents a simpler solution to one aspect of the provider enrollment process.
Many commercial carriers utilize CAQH to obtain credentialing information from a central location and require that providers have a complete and up to date profile in the CAQH system as part of the enrollment process. Learn how a large regional health plan has dramatically increased EFTERA enrollment for all providers in their network while reducing errors and provider abrasion. To self register complete the form in its entirety and click the Continue button.
Change Enrollment Requested. CAQH is a non-profit alliance of health plans and related associations working together to streamline the business of healthcare. CAQH is a non-profit alliance of health plans and related associations working together to streamline the business of healthcare.
Ace New CAQH Proview Changes and Speed Enrollment. The system eliminates duplicative processes to collect provider demographic. If you have been invited to the CAQH ProView TM via a Participating Organization please click the hyperlink.
The provider user submitted a change to an existing enrollment. Your organization can use CAQH ProView to streamline all processes requiring provider demographic data including claims administration directory services credentialing and more. The CAQH Universal Provider Datasource is designed to be compliant with all laws rules and regulations relating to the privacy of individually identifiable health information.
CAQH has developed a simple cost-effective solution to help health plans move closer to universal EFT. Single Sign-on for Dentists. CAQH has verified the enrollment information.
Sign in on the right to update your existing profile information or if you are a new provider to CAQH ProView register to create a profile. CAQH is verifying the information. Health plan application.
Yesenia Servin CPMSM PESC. CAQH ProView is more than a credentialing database. Explore CAQH Solutions for provider credentialing and verification directory maintenance coordination of benefits and more.
CAQH ProView is the healthcare industrys premier resource for self-reporting professional and practice information to health plans and other healthcare organizations. Provider Enrollment or Payor Enrollment refers to the process of applying to health insurance networks for inclusion in their provider panels. CAQH ProView Provider User Guide v30.
60-90 minutes each Expert. Plans have resigned themselves to sending checks or using expensive payment vendors for the remainder.
