During this time you can still find all forms and guides on our legacy site. A library of the forms most frequently used by health care professionals.
Https Www11 Anthem Com Ca Provider F1 S0 T0 Pw E229275 Pdf Refer Provider
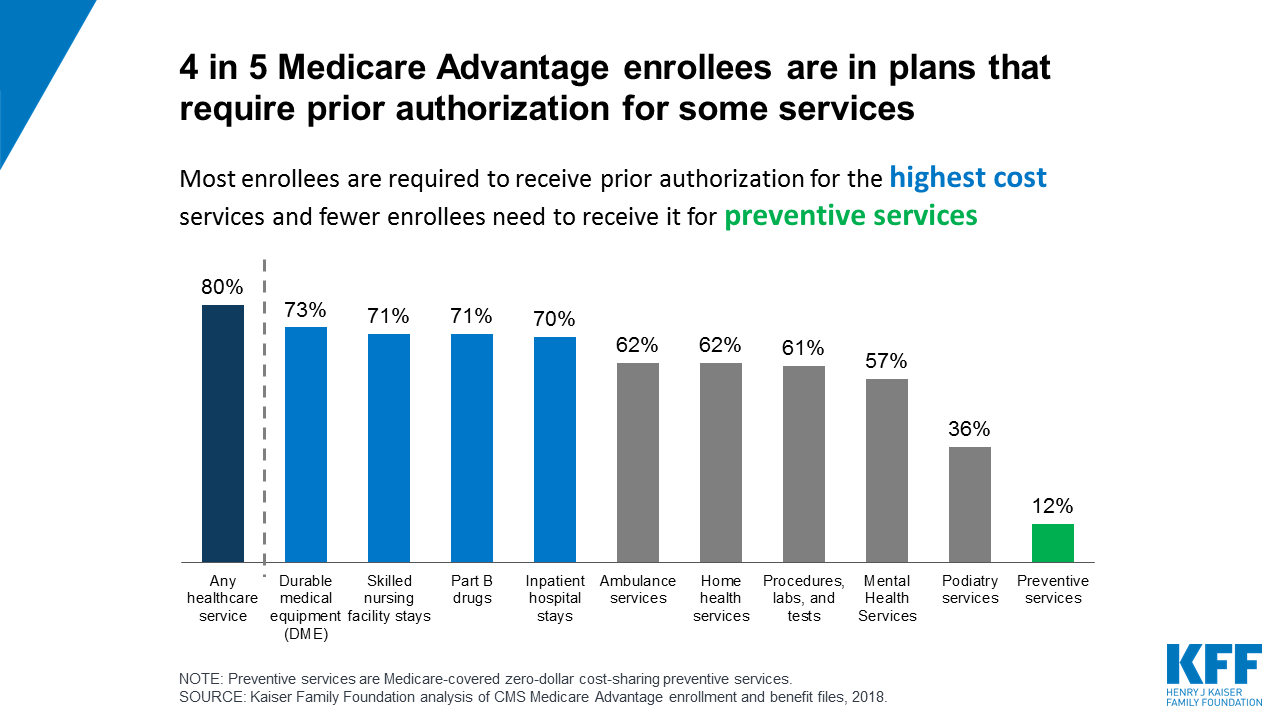
This process is called prior authorization.
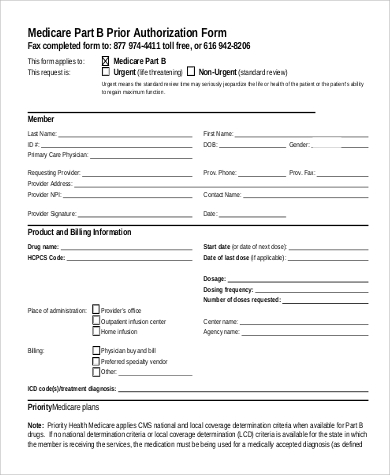
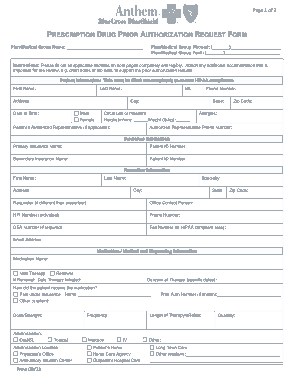
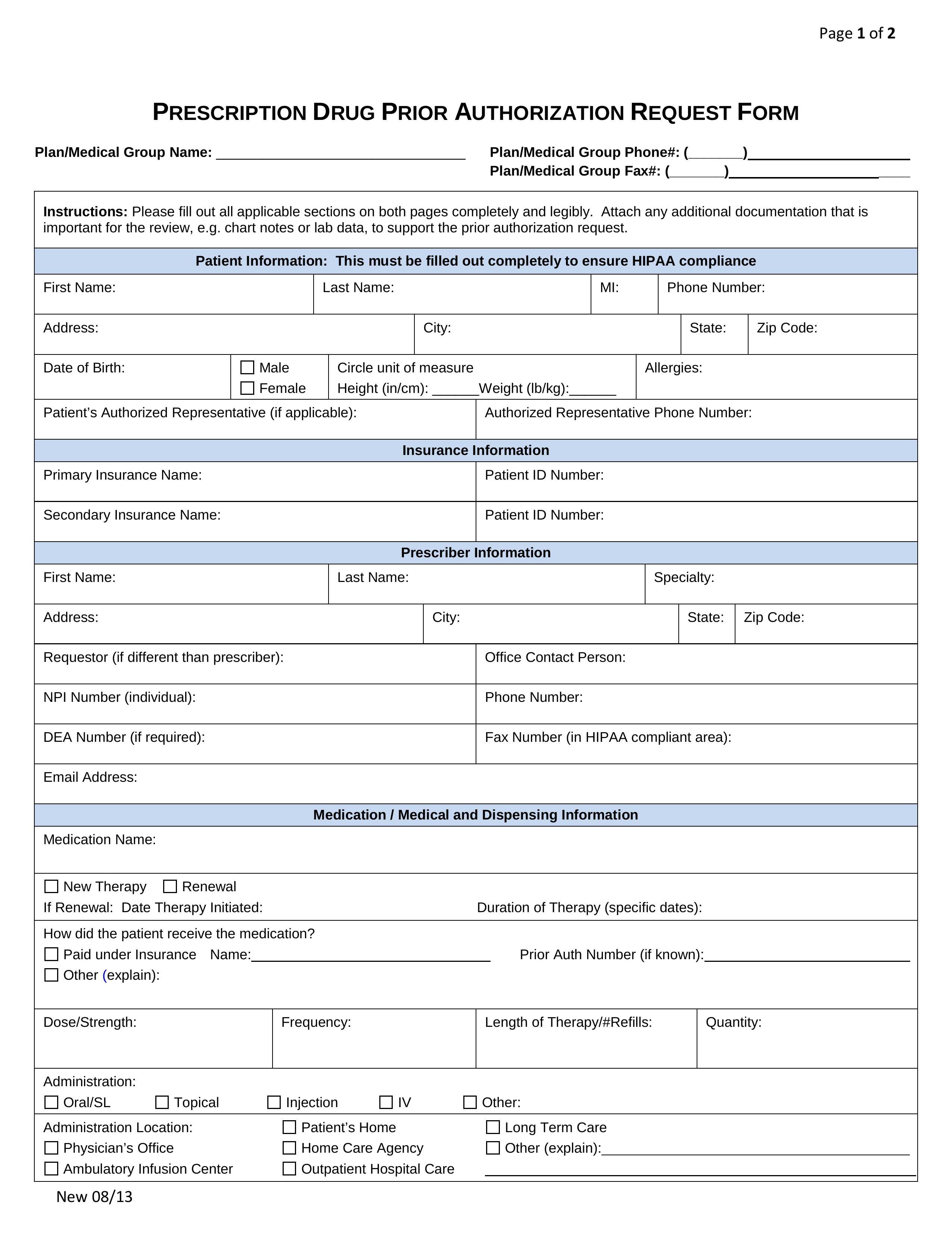
Anthem bcbs prior authorization form pdf. Prior authorization focuses on drugs that may have a. Providers are strongly encouraged to verify that a prior authorization has been obtained before scheduling and performing services. Complete Anthem Prior Authorization Request online with US Legal Forms.
Medicare Prior Authorization Review. Provide this information in the. Weve provided the following resources to help you understand Anthems prior authorization process and obtain authorization for your patients when its required.
Please complete ALL information requested on this form incomplete forms will be returned to sender. 711 24 hours a day 7 days a week or through our website at. 800 714-0040 Monday-Friday 7 am-7 pm.
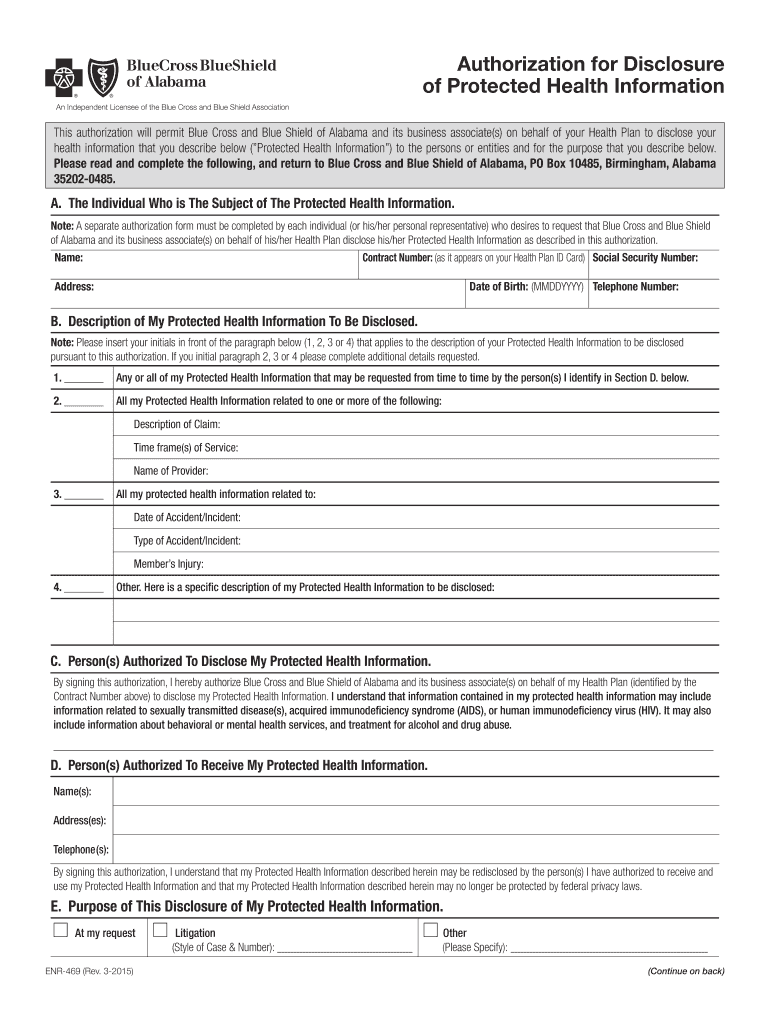
Health insurance can be complicatedespecially when it comes to prior authorization also referred to as pre-approval pre-authorization and pre-certification. Anthem Blue Cross and Blue Shield Indiana Medicaid Prior Authorization Requirements Page 2 of 2 Detailed vendor information The Precertification Lookup Tool can be used to look up specific codes for additional detailed vendor information. Adobe PDF The Anthem Blue Cross Blue Shield prior authorization form is a simple document used to request a non-formulary drug for a patient and member of Anthem Blue CrossBlue.
PF-AIN-0011-15 April 2015 Instructions 1. But some drugs need to be reviewed by your health plan before theyre covered. Independent licensees of.
Anthem Blue Cross Blue Shield Prior Rx Authorization Form PDF The Anthem Blue Cross Blue Shield prior authorization form is what physicians will use when requesting payment for a. We review requests for prior authorization based on medical necessity only. Important for the review eg.
Prior Authorization Clinical Edits for the National Drug List Most prescriptions are filled right away when you take them to the pharmacy. You will be happy to know that we have added additional requirements to make it easier for you when submitting prior authorization. The Blue Cross and Blue Shield names and symbols are registered marks of the Blue Cross and Blue Shield Association.
Prior Authorization Lookup Tool. Providers can call the AIM Contact Center toll-free number. Anthem Blue Cross and Blue Shield Prior Authorization Form for Medical Injectables Page 2 of 2 I certify that the information provided is accurate and complete to the best of my knowledge and I understand that any falsification omission or concealment.
In addition to commercial issuers the following public issuers must accept the form. Anthem UM Services Inc. Save or instantly send your ready documents.
The forms in this online library are updated frequentlycheck often to ensure you are using the most current versionsSome of these documents are available as PDF files. We are currently in the process of enhancing this forms library. If you do not have Adobe Reader download it free of charge at Adobes site.
Easily fill out PDF blank edit and sign them. Anthem HealthKeepers Plus Pharmacy Prior Authorization Form Page 2 of 3 Medication information Drug name and strength requested SIG dose frequency and duration HCPCS billing code Diagnosis andor indication ICD code Has the member tried other medications to treat this condition. As of October 1 2018 you should be utilizing the new Anthem Blue Cross Anthem prior authorization form for MediCal Managed Care and LA.
Medicaid the Medicaid managed. San Antonio TX 78265-8686. Click the link to open the form in a new browser window then use your browsers Print button to.
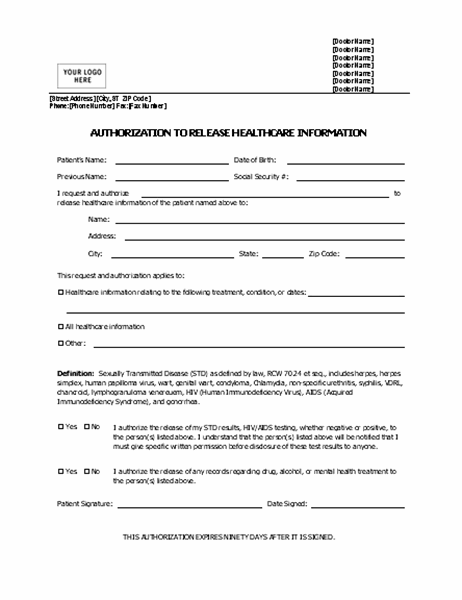
Anthem Blue Cross is the trade name of Blue Cross of California and Anthem Blue Cross Partnership Plan is the trade name of Blue Cross of California Partnership Plan Inc. Information contained in this form is Protected Health Information under HIPAA. Chart notes or lab data to support the prior authorization or step-therapy exception request.
PREAUTHORIZATION FAX FORM If Urgent request please call Anthem If Urgent request please call Anthem Instructions. Complete this form in its entirety. Any incomplete sections will result in a delay in processing.
Prior Authorization Health insurance can be complicatedespecially when it comes to prior authorization also referred to as pre-approval pre-authorization and pre-certification. Date range of use Yes. Easily find and download forms guides and other related documentation that you need to do business with Anthem all in one convenient location.
Weve provided the following resources to help you understand Empires prior authorization process and obtain authorization. You may also ask us for a coverage determination by phone at Anthem Blue Cross Cal MediConnect Plan Medicare-Medicaid Plan Pharmacy Member Services 1-833-214-3606 TTY. Beginning September 1 2015 health benefit plan issuers must accept the Texas Standard Prior Authorization Request Form for Health Care Services if the plan requires prior authorization of a health care service.