Remember if you sign up on day 59 you will have to pay retroactive premiums. However the act does not require them to pay for it.
 How To Read Your Insurance Card University Of Utah Hospitals Clinics University Of Utah Health
How To Read Your Insurance Card University Of Utah Hospitals Clinics University Of Utah Health
However dependents can receive up to 36 months of coverage if you switch to Medicare get divorced or die.

Cobra health insurance card. Both cards offer equal access to necessary healthcare. Ad Enhance Your Wellbeing Strategy And Tackle Absenteeism With A Health Plan. Attract The Best Talent By Implementing An Employee Rewards Strategy.
COBRA Insurance Knowledge Base General insurance information provided on COBRA Insurance Website is not intended to substitute for informed professional medical psychological tax legal investment accounting governmental or other professional advice. Under COBRA youll have to pay the full premium for your coverage plus an administrative fee. Your cost can be up to 102 of the total cost of the premium with the extra 2 labeled an administrative fee.
COBRA stands for Consolidated Omnibus Budget Reconciliation Act. Are you my new insurance carrier. Buy insurance before travelling.
Ad Enhance Your Wellbeing Strategy And Tackle Absenteeism With A Health Plan. Most carriers do not issue new ID cards for COBRA coverage and your member ID number will generally remain the same under COBRA. 1 Before deciding whether you should sign up for COBRA there are pros and cons to consider and important steps to take to make sure you get coverage in time.
Your Health Insurance Card. COBRA requires employers to keep you on their insurance for as long as you need it or for the maximum time frame. When youre employed your employer generally pays for some of the cost of your health insurance.
Buy insurance before travelling. View Our Cash Plans. The Consolidated Omnibus Budget Reconciliation Act COBRA is a health insurance program that allows eligible employees and their dependents the continued benefits of.
You will not be able to tell from the insurance card if the payments are made under COBRA or not. Ad European and Global Health Insurance Cards are valid for travel in the EU. Ad European and Global Health Insurance Cards are valid for travel in the EU.
You do not have to be unemployed to have insurance under COBRA. Can I elect COBRA. Attract The Best Talent By Implementing An Employee Rewards Strategy.
Ad Compare Award-Winning Health Care Providers And Ensure Your Health Is In Safe Hands. COBRA lets you extend your former employers health plan. COBRA coverage begins the date your health insurance policy ends because of a qualifying event.
It is recommended that you contact your insurance carrier directly with any questions regarding claim issues or what is covered under your benefit plan. Ad Compare Award-Winning Health Care Providers And Ensure Your Health Is In Safe Hands. That means youll likely be paying more for COBRA and it may get expensive depending on the kind of coverage you have.
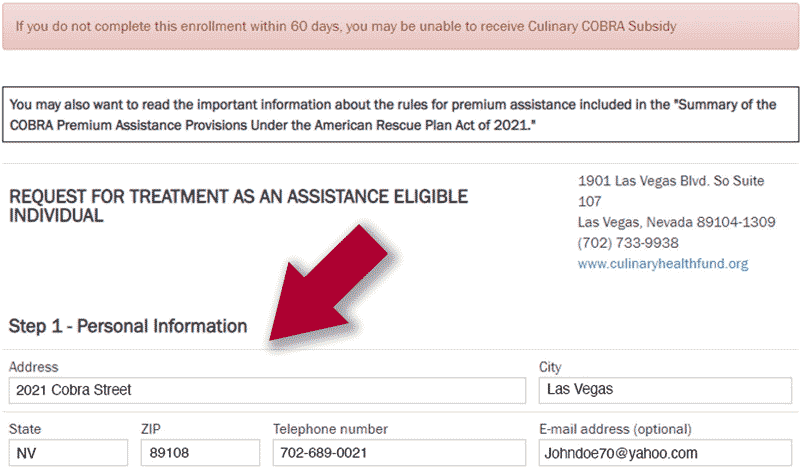
Cover Medical Expenses For Illness Injuries When You Buy Health Care Insurance With Us. For an employee covered under a qualifying event COBRA coverage can last for 18 months from the date you elect coverage. You have 60 days to decide whether to sign up for COBRA.
If you find yourself unemployed and worried about your options for a good health insurance plan COBRA is one choice that allows you to continue your employee health insurance benefits even if you no longer work for your last employer. COBRA Simple is the third-party COBRA administrator and we are not associated with the insurance companies in any way. Its a federal law that was created in 1985 that gives individuals who experience a job loss or other qualifying event the option to continue their current health insurance coverage for a limited amount of time.
Cover Medical Expenses For Illness Injuries When You Buy Health Care Insurance With Us. COBRA requires you to pay 100 of the health insurance costs plus up to 2 adminstrative fee. COBRA is a provision that states that employer must allow you access to keep the same plan for the next 6 month as long as you pay the entire premium your own the employer contribution.
Both cards offer equal access to necessary healthcare. View Our Cash Plans. Unless youve lost your insurance card the same one you had should still work.
The old card will be re-activated once your employer has received your COBRA payment. Since COBRA insurance is continuation of your previous employers group health policy you will be able to use the same ID cards.