QB has 45 days from the. QB has 60 days from the date of notice or the date of loss of coverage whichever is later to elect COBRA.
Cobra Qualifying Events 24hourflex
QB has 60 days from the date of notice or the date of loss of coverage whichever is later to elect COBRA.
Cobra enrollment timeline. A beneficiary who receives a COBRA election notice ordinarily has 60 days following receipt of the notice or other qualifying event whichever is later to elect COBRA continuation coverage. IC has 14 days to send a COBRA packet to QB. Timeline for COBRA enrollment Employee andor dependent COBRA qualifying event QB has 30 days to notify their employer.
The COBRA subsidy will begin for coverage periods beginning on April 1 2021 and ending on September 30 2021. The Consolidated Omnibus Budget Reconciliation Act COBRA gives workers and their families who lose their health benefits the right to choose to continue group health benefits provided by their group health plan for limited periods of time under certain circumstances such as voluntary or involuntary job loss reduction in the hours worked transition between jobs death divorce and. For ERISA claims deadlines.
Your dependents a COBRA enrollment form. If an employee or dependent chooses to terminate COBRA coverage early with no special enrollment. The member has 60 days from the postmark date on the COBRA Specific Rights Notice Letter to elect coverage.
To notify their employer. To send a COBRA packet to QB. COBRA Timeline Day 1.
Timeline for COBRA enrollment. Anyone eligible for COBRA insurance benefits has 2 months following the date of the end of their coverage or the day they receive a COBRA notification to enroll in a COBRA coverage plan. To exhaust COBRA continuation coverage you or your dependent must receive the maximum period of continuation coverage available without early termination.
In other words COBRA premiums would be covered at 100 for assistance eligible individuals AEI as defined under the Act from April 1 2021 through September 30 2021. Boards. Office of Management and Enterprise Services.
For HIPAA special enrollment rights the 30- or 60-day time period to make election changes. Boards. Your deadline is 90 days from enrollment on a COBRA plan.
This includes an employee and covered spouse. Office of Management and Enterprise Services. The event date is the date on which an employee experiences a COBRA-qualifying event.
Enrollment event such as marriage the birth of a child or if you exhaust your continuation coverage. COBRA enrollees normally have 45 days from their COBRA election to make the first premium payment and subsequent monthly payments must be made within a 30-day grace period that starts at the. If the employer requires the COBRA beneficiary to pay a premium which premium may not exceed 102 of the total premiums paid for or by other similarly situated plan beneficiaries the beneficiary has an additional 45 days after electing coverage to pay the initial premium under COBRA.
Within 30 days of losing COBRA coverage for coverage through another group health plan or Within 60 days before or after losing COBRA coverage for coverage through a Marketplace plan. From the election date to pay full premiums directly to EGID. You andor your dependents have 45 days after making your election to pay back premiums.
Employee andor dependent COBRA qualifying event. The date for individuals to notify the plan of COBRA qualifying events such as divorce or disability. You andor your dependents have 60 days after the event or date the COBRA enrollment form was sent whichever is later to elect COBRA coverage and return your enrollment form.
Establish an internal process wherein you are notified of any new active plan enrollments. The 30-day grace period for a COBRA qualified beneficiary to make monthly premium payments ongoing payments. If a spouse is added later you will need to be notified.
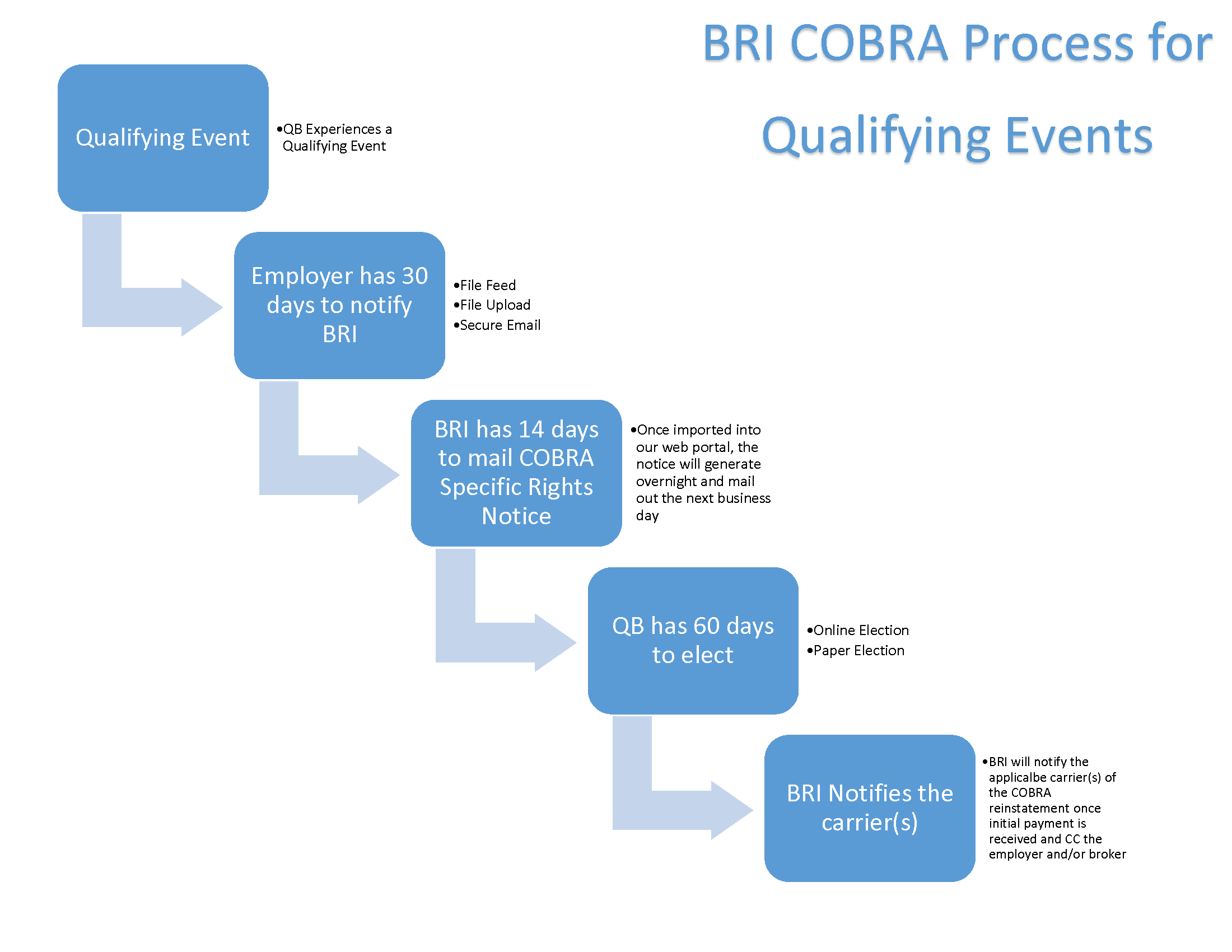 The Next Step What Happens When A Qualifying Cobra Event Occurs Bri Benefit Resource
The Next Step What Happens When A Qualifying Cobra Event Occurs Bri Benefit Resource
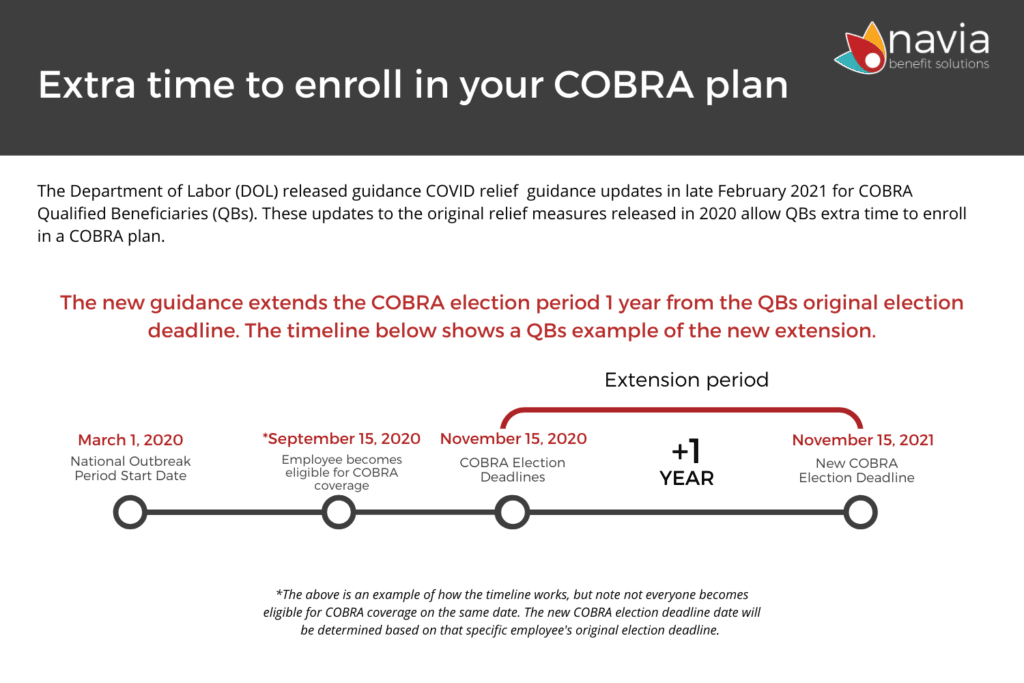 Cobra Subsidies Fsa Dependent Care Increase And Benefit Extensions From Arpa Navia
Cobra Subsidies Fsa Dependent Care Increase And Benefit Extensions From Arpa Navia
Cobra Management Services Denver Blog Cobrahelp
 Cobra Subsidy Confusion Ehealthinsurance Answers Questions And Releases Cobra Subsidy Timeline Chart Ehealth
Cobra Subsidy Confusion Ehealthinsurance Answers Questions And Releases Cobra Subsidy Timeline Chart Ehealth
Https Www Nbsbenefits Com Documents Fee Schedules Cobrabrochure Pdf
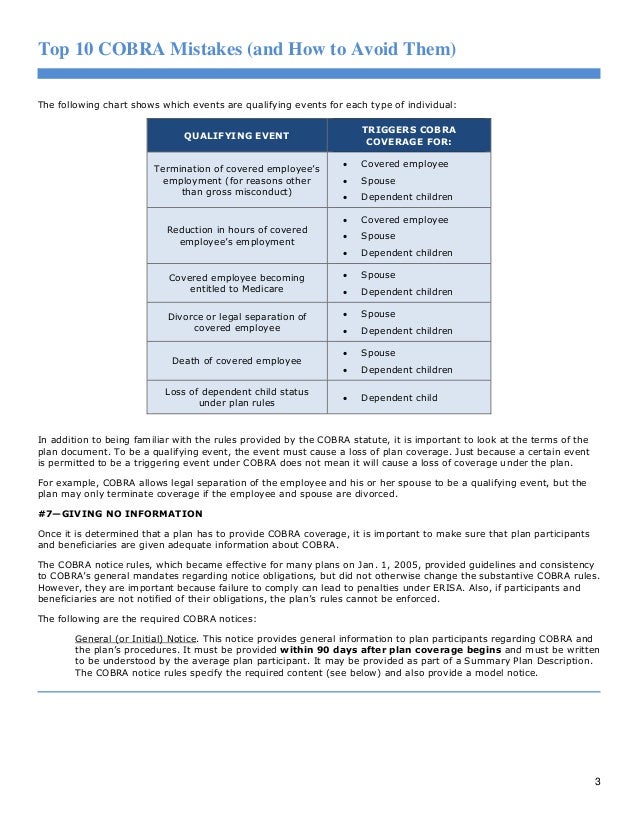 Top 10 Cobra Mistakes And How To Avoid Them
Top 10 Cobra Mistakes And How To Avoid Them
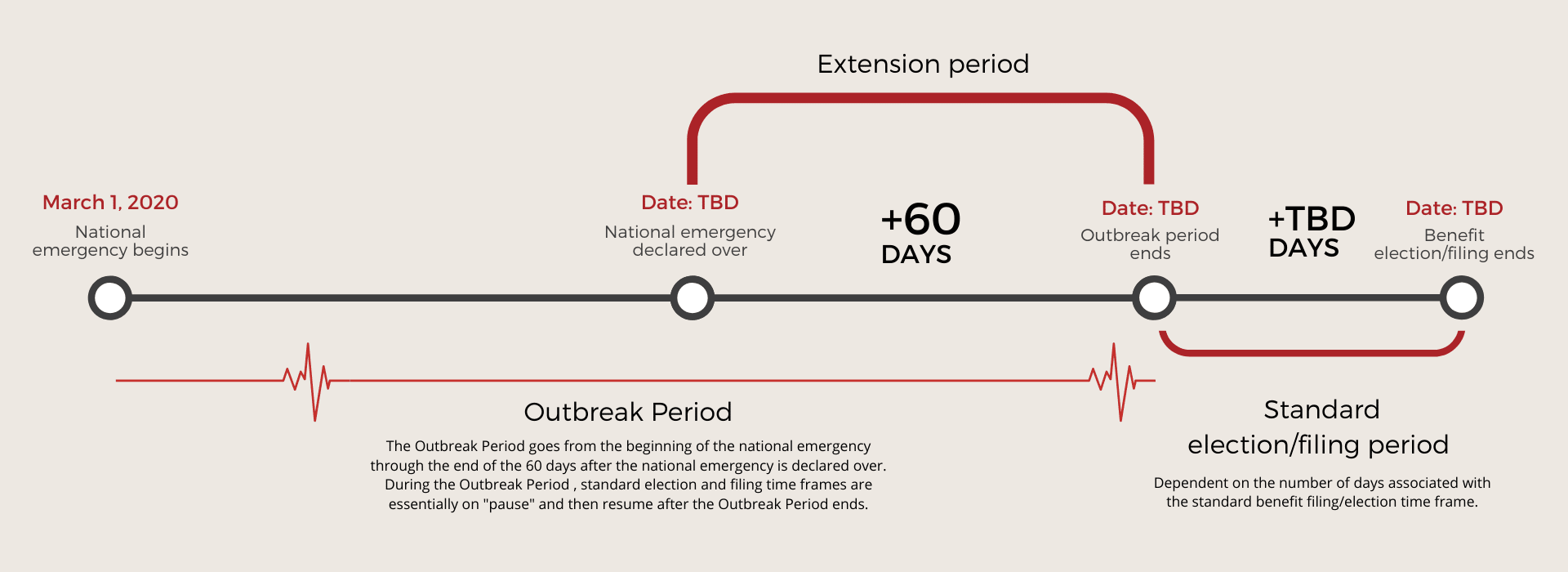 Employee Benefit Extensions For The Covid 19 Pandemic Cobra Fsa Hra And More Navia
Employee Benefit Extensions For The Covid 19 Pandemic Cobra Fsa Hra And More Navia
Benefits Administration Solutions
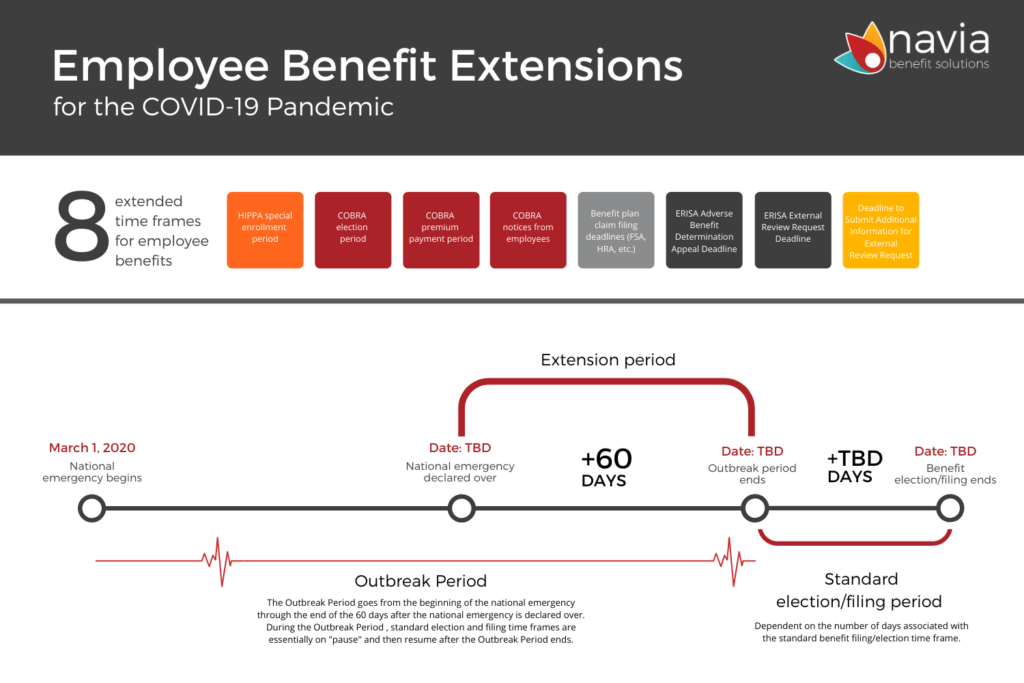 Employee Benefit Extensions For The Covid 19 Pandemic Cobra Fsa Hra And More Navia
Employee Benefit Extensions For The Covid 19 Pandemic Cobra Fsa Hra And More Navia
Https Www Wageworks Com Media 107859 Ww Cobra Admin Guide 062410 Pdf
Https Www Nbsbenefits Com Wp Content Uploads 2015 12 Cobra Employer Manual Pdf
 Major Changes To Special Enrollment And Cobra Timeframes Hays Companies
Major Changes To Special Enrollment And Cobra Timeframes Hays Companies
 Cobra Subsidies In Covid 19 Rescue Plan Require Employer Action Mercer
Cobra Subsidies In Covid 19 Rescue Plan Require Employer Action Mercer

No comments:
Post a Comment
Note: Only a member of this blog may post a comment.