These procedures are usually covered by medical insurance and there are no costs after the surgery is done. A letter of medical necessity is a letter provided by your local doctor describing what your symptoms are what your diagnosis is and why a reversal surgery is medically required.
They feel the same about paying for infertility treatment if you have had a voluntary tubal ligation procedure.
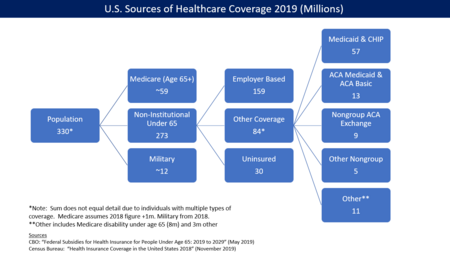
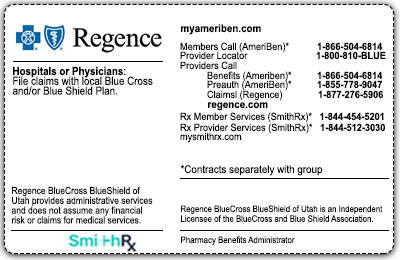
Does insurance cover tubal ligation. The cost of other birth control methods such as pills or condoms and spermicide may be greater over time. In case the insurance. Insurance companies that typically cover tubal ligation include Aetna United Healthcare CignaSagamore and Anthem BlueCross BlueShield.
In some cases a tubal ligation can result in medical issues. They will not pay for breast augmentations face lifts tummy tucks etc. Contrary to tubal ligation vasectomy rates tend to increase with more education and higher socioeconomic status and so are more common among men covered by private insurance.
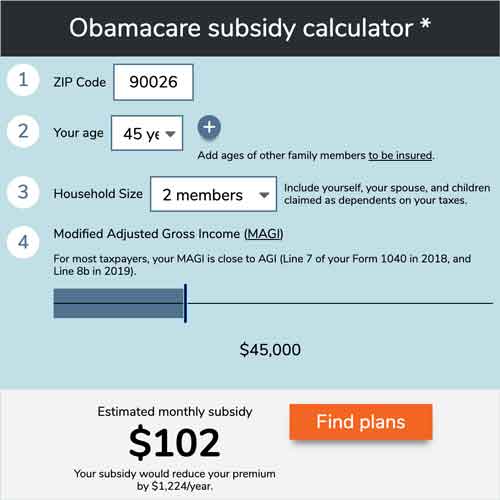
Although tubal ligation and tubal implants are expensive it is a one-time cost. When a procedure is requested out of medical necessity the chances for insurance approval rise. Shared cover means you and Southern Cross each pay some of the costs.
Sometimes they will add to your monthly or annual fee that will end up costing you more in the long run. Youre not being cheap by asking your insurance company to cover a part of your tubal ligation reversal. Although tubal ligation and tubal implants are expensive it is a one-time cost.
Regarding this what does Southern Cross cover. Pregnancy termination is covered only as specified in AMPM Policy 410 including Mifepristone Mifeprex or RU-486. This means that neither a tubal ligation via salpingectomy or a salpingectomy billed under 58700 or 58661 can be covered 100 as sterilization under the ACA.
The doctor may also completely remove the fallopian tubes. Some will pay for IVF but will not do it if you have had a voluntary tubal ligation. If your insurance company doesnt cover a tubal ligation via salpingectomy as sterilization and hasnt updated their bulletins to cover 58700 or 58661 as sterilization.
Unfortunately many insurance cos that typcially cover IVF will not if there has been voluntary sterilization. A tubal ligation works immediately but requires a general anaesthetic and a hospital stay. If your doctor feels that your tubal ligation should be completed for your health he can write a letter to the insurance companies and make the case for medical necessity.
Is anyone able to explain why my insurance UHC will pay 100 to have my tubes cut and cauterized but they will not pay to have them cut and removed entirely. The cost of other birth control methods such as pills or condoms and spermicide may be greater over time. To close your tubes the doctor may band burn cauterize tie and cut or clip them.
Its also called having your tubes tied. Emergency contraceptionPlan B Ella and Next Choice Your plan may also cover. After this an egg cant move down your tubes and cant be fertilized.
These procedures are usually covered by medical insurance and there are no costs after the surgery is done. However things can go wrong and these complications are often a covered medical reason. Because sterilisation is an elective procedure vasectomies and tubal ligation are typically covered under higher-tier hospital policies.
Why does insurance cover tubal ligation 100 but not salpingectomy complete removal of tube. Permanent contraception methods such as tubal ligation often called getting your tubes tied. Many do have appeals processes though.
Some insurance providers cover the surgery as a portion of their plan. It is more likely that your Medical or private insurance policy will cover any complications arising from your tubal reversal operation. Check your health insurance product disclosure statement PDS or contact your fund to find out if your policy covers it.
This is viewed as an elective procedure and elective procedures by definition arent medically necessary. This means you cant get pregnant. Consequently does insurance cover tubal ligation.
Don Snyder an Indiana gynecologist. Moreover does my insurance cover tubal ligation. The surgery is very safe.
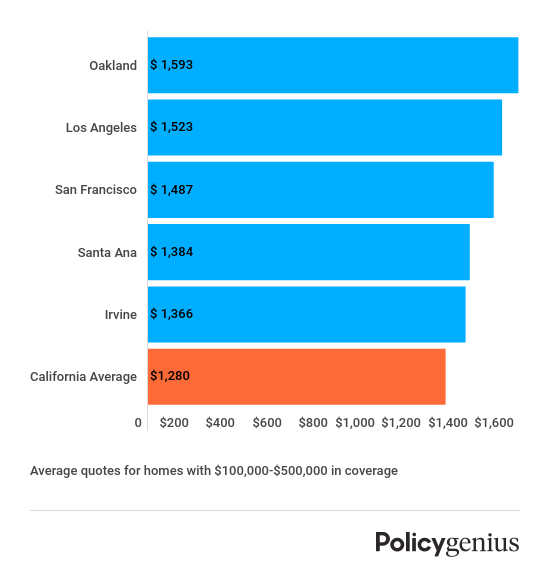
Sterilization services are covered for both male and female members when the requirements specified in this Policy for sterilization services are met including hysteroscopic tubal sterilizations and e. The cost of a tubal ligation varies and depends on where you get it what kind you get and whether or not you have health insurance that will cover some or all of the cost. Most health insurances will not pay for non-essential surgery.
Your level of cover. It is highly unlikely that your insurance carrier will cover the reversal of a tubal ligation. Is it because youre technically sterile by just snipping them so removing entirely is seen as.
Sometimes your health insurance company will say they will pay for tubal reversal surgery but only if a doctor provides a letter of medical necessity. Tubal ligation may be totally free or low cost with some health insurance plans Medicaid and other government programs. Tubal ligation typically is covered by most health insurance according to Dr.
Some insurance providers insure artificial insemination and you must check with your insurance whether they cover it. Many insurance providers do not cover tubal reversals. Tubal ligation is surgery to close your fallopian tubes.
The plan provides a contribution towards cancer care surgical procedures consultations 1 diagnostic imaging tests recovery and day-to-day healthcare.