Even if their COBRA is not approved until 5 20 or some later date they still have COBRA coverage from 51 and can submit claims for care expenses that occur between 51 and 5 20. Retiree Health Coverage Offered by a Former Employer Those that are offered retiree health coverage may be considered for premium assistance.
.jpg?width=850&height=566) Health Care Options Cobra Vs Individual Coverage On Covered California Word Brown
Health Care Options Cobra Vs Individual Coverage On Covered California Word Brown
If you already chose COBRA you can cancel it.
.jpg?width=850&height=566)
Can i get covered california instead of cobra. The new Affordable Care Act health plans offered through Covered California will help many people move out of an expensive COBRA plan and into an insurance plan with lower premiums. You can choose Covered California instead of COBRA. You dont have to wait for your current coverage to end.
If you qualify you should get a written notice of your eligibility for COBRA. The formulary is smaller on Covered California plans so if you have medications now check with us first. When does the COBRA subsidy end.
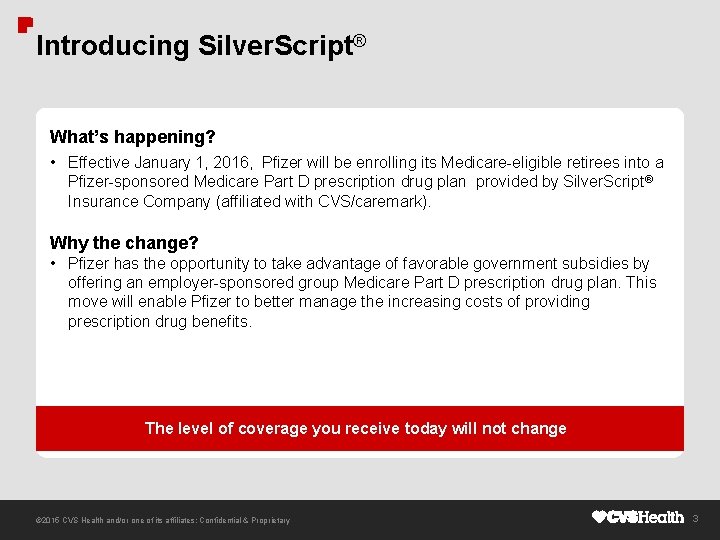
If youre eligible for COBRA because of a reduction in the hours you work or you involuntarily lost your job you may qualify for help paying for your COBRA premiums called premium assistance from April 1 2021 through September 30 2021 under the American Rescue Plan Act of 2021 based on how long your COBRA coverage can last. My Medi-Cal has been discontinued and I am now able to enroll in Covered California during a Special Enrollment Period SEP how can I avoid a gap in my health coverage. You may be eligible to apply for individual coverage through Covered California the States Health Benefit Exchange.
You must apply by December 15 2017 for your coverage to begin on January 12018. When would I need to sign on with Covered CA if my job and coverage ends on 12312019. In order t take advantage of the special enrollment in Covered California.
This is the other consideration along with doctor networks. If someones Medi-Cal coverage is cancelled due to increased income or decreased household size does that person qualify for special enrollment into Covered California. You must apply by December 15 2019 for your coverage to begin on January 12020.
These individuals are known as qualified beneficiaries. Conversely continuing group coverage through COBRA is often more expensive than Individual plans via Covered California. Can I get covered under Covered CA instead.
Employees who are offered health coverage by their employer that is affordable and that meets minimum value standards are not eligible for financial help to help pay premiums for an individual Covered California health plan. What about Cobra versus Covered California for RX. The formulary list of drugs is different between group plans Cobra and individual family plans Covered Ca.
However if an individual declines the initial offer of COBRA heshe may qualify for special enrollment in Covered California health insurance or an off-exchange plan outside of the annual Open Enrollment period for IndividualFamily coverage. The terms and timeframes are set by the Department of. This is because individual plans often have different network options of providers and can offer an array of different health costs for services especially for deductibles coinsurance etc.
Before doing this keep in mind these guidelines. In California if your employer has two to 19 employees you may be covered by Cal-COBRA. Cal-COBRA may also be able to extend your coverage if your federal COBRA plan has expired.
You must apply by December 15 2017 for your coverage to begin on January 12018. Their COBRA election window begins on 51. The COBRA subsidy ends for everyone on September 30 2021.
There is no need for COBRA. Generally premium assistance means that youll have a 0 monthly premium. You can buy a Covered California health plan but you will have to pay the full cost without tax credits.
You dont have to wait for. Most consumers will pick either COBRA or Covered California but some may need to pick both to avoid a gap in coverage. Be aware that if you are already enrolled on COBRA you cannot switch onto a health plan through Covered California until the next open enrollment period.
For covered individuals whose initial COBRA eligibility period began before April 1 eligibility for the COBRA subsidy will end before September 30 if their original 18- or 36-months of COBRA eligibility ends before September 30. So long as they enroll in COBRA within the election period theyll be covered by COBRA from 51 on. The COBRA statute requires employers to offer continuation of group coverage eg medical dental and vision to covered employees spouses domestic partners and eligible dependent children who lose group coverage due to a qualifying event.
Because of this many people and families on or. If you enroll in a Covered California plan and make a payment before your employer coverage ends Covered California will pick up where your employer coverage leaves off. The key advantage of this alternative to COBRA is that you can quickly apply and get approved.
Under COBRA there are often no cost-sharingpremium assistance options available and coverage can. You have the option of getting short-term health insurance to cover the lapse between your current insurance and the insurance you will get from your new employer. What can I do when my Federal COBRA or Cal-COBRA options have been exhausted.
In other words the ARPAs COBRA subsidy provisions do not extend the period of COBRA. However COBRA is considered employer offered health insurance that meets minimum essential benefits and value. You can choose Covered California instead of COBRA.
An off-exchange plan are plans that are offered by the carrier direct rather than through Covered California. It takes as little as 30 seconds to get a quote for a short-term plan online and coverage often.