When we review certain drugs before your plan covers them it helps. If you need assistance call 850 412-4166.
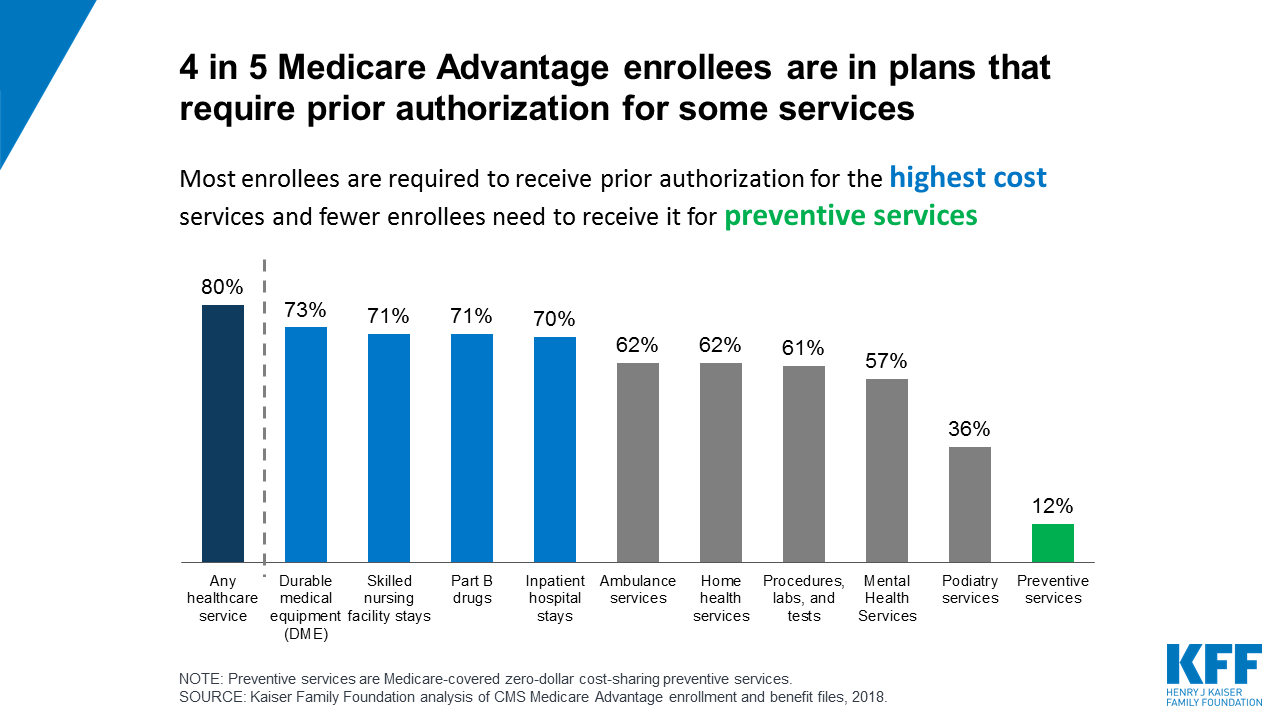 Prior Authorization In Medicare Advantage Plans How Often Is It Used Kff
Prior Authorization In Medicare Advantage Plans How Often Is It Used Kff
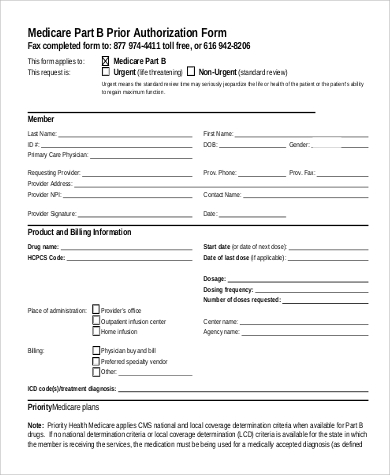
Part B pharmacy prior authorization drug requests All other medical prior authorization requests If you want your requests to process faster make sure youre using the right form and faxing it to the correct department.
Medicare pharmacy prior authorization. In order to obtain copies of prior authorization forms please click on the name of the drug requiring prior authorization listed below. Fill out Authorization to Disclose Personal Health Information. Once a patient or their physician receives a written denial coverage determination they should submit a coverage determination request form asking for the drug to be covered.
M or F Contact Person at Doctors Office. To get the Medicare form you need find the situation that applies to you. Thats not always the case.
Pharmacy supplies drug. This form is available both in English. This tool is used by ODM to ensure safety of our beneficiaries and to help control costs.
The Health Plan will notify you of its prior authorization decision via fax on the date the actual decision is made. You can find both forms on our Medicare Advantage forms page. The Medicare Prior Rx Authorization Form or Drug Determination Request Form is used in situations where a patients prescription is denied at the pharmacy.
If your office is unable to receive faxes you will be notified via US. TTY 1-877-486-2048 Mailing address. Prior authorization is a requirement that a health care provider obtain approval from Medicare to provide a given service.
Additionally requests that are subject to prior authorization or any other utilization management requirement may require supporting information. Prior authorization PA is the process of obtaining additional information from the prescriber of a procedure medication or service for the purpose of ensuring eligibility benefit coverage medical necessity location and appropriateness of services. The full list of HCPCS codes requiring prior authorization is available here PDF.
Pharmacy Prior Authorization Forms Preferred Drug List Health Resources. If you want Medicare to be able to give your personal information to someone other than you you need to fill out an Authorization to Disclose Personal Health Information Get this form in Spanish. When your doctor prescribes a medication you trust its the right one for you.
Forms for state mandates. Date Faxed to MD. If you do not see the name of the drug needing prior authorization listed below you will need to select the Miscellaneous Pharmacy Prior Authorization Request form.
I want to make sure Medicare can give my personal health information to someone other than me Authorization to Disclose Personal Health Information formCMS-10106. Prior Authorization is about cost-savings not care. And thats why we have programs like prior authorization.
Medicare Contact Center Operations PO Box 1270 Lawrence KS 66044. Private for-profit plans often require Prior Authorization. The Pharmacy Services call center accepts requests for prior authorization over the phone at 1-800-537-8862 between 8 AM and 430 PM Monday through Friday.
Medicare Advantage MA plans also often require prior. Clinical documentation supporting the medical necessity of the prescription must be submitted to the Department for all prior authorization requests. 7231 Parkway Drive Suite 100 Hanover MD 21076.
Diagnosis and Medical Information. Complete the applicable form below and fax it to 1-855-681-8650. Get forms in alternate formats.
They can also fax our prior authorization request form to 855-637-2666. A request must be submitted and approved in advance for medications. To request prior authorization you or your provider can call Moda Health Healthcare Services at 800-592-8283.
Formulary ExceptionPrior Authorization Request Form Patient Information Prescriber Information Patient Name. If you require a prior authorization for a medication not listed here please contact UPMC Health Plan Pharmacy Services at 1-800-979-UPMC 8762. Puerto Rico prior authorization.
Under Prior Authorization benefits are only paid if the medical care has been pre-approved by Medicare. 410 424-4607 or 410 424-4751. 2020 Request for Medicare Prescription Drug Coverage Determination Page 1 of 2.
When we say you need to get prior authorization for a service or prescription drug it means that you need to get pre-approval from us to cover it. If your pharmacist said your prescription drug needs our approval this explains why and what your options are. Please attach supporting information as necessary for.
Pharmacy Prior Authorization Form. These two services will be in addition to the existing list of services requiring prior authorization which include blepharoplasty botulinum toxin injection rhinoplasty panniculectomy and vein ablation. Prior authorization for pharmacy drugs Submitting a request for prior authorization.
FAX FAX Completed Form AND APPLICABLE PROGRESSCompleted Form AND APPLICABLE. Congress Considers Fixes For Medicare Advantage Prior Authorization A bill that would speed up the prior authorization process and demand more transparency when insurance plans deny health.