This plan provides limited benefits. NGAH_TRIOMED_AGENTTRAINING 32021 2021 National Health Insurance Company.
 National General Insurance Review 2020 Insurance Blog By Chris
National General Insurance Review 2020 Insurance Blog By Chris
Term Life Only Brochure.

National general triomed. It helps you get well without worrying about medical bills piling up. Non-ST elevation myocardial infarctions NSTEM are NOT covered. National Generals entire portfolio of short term and supplemental insurance can be sold year-around.
The benefit amount is reduced to 10 of the maximum allowed benefit if diagnosis occurs within first 90 days. Select Dental PPO Brochure Flyer. National General makes it easy for you to find sales success.
TrioMed enthält eine starke antimikrobielle Substanz um mikrobiologische Kontamination zu verhindern Bakterien Viren Sporen. Thank you for being a National General Insurance customer. Plan Enhancer Brochure Flyer.
Return to National General Information Page. Simply choose the desired benefit maximum once and coverage is extended to all TrioMed covered benefits. National General Foundation Health Brochure.
For glass only claims please call 1-800-468-3466. REQUEST A National General CONTRACT. National General Plan Enhancer.
TrioMED A plan for unexpected out-of-pocket costs associated with accidents critical illnesses and accidental death National General Accident and Health markets products underwritten by National Health Insurance Company Time Insurance Company Integon National Insurance Company and Integon Indemnity Corporation. TrioMed Brochure Spanish A plan for unexpected out-of-pocket costs associated with accidents critical illnesses accidental death and dismemberment. CRITICAL ILLNESS - TERM LIFE.
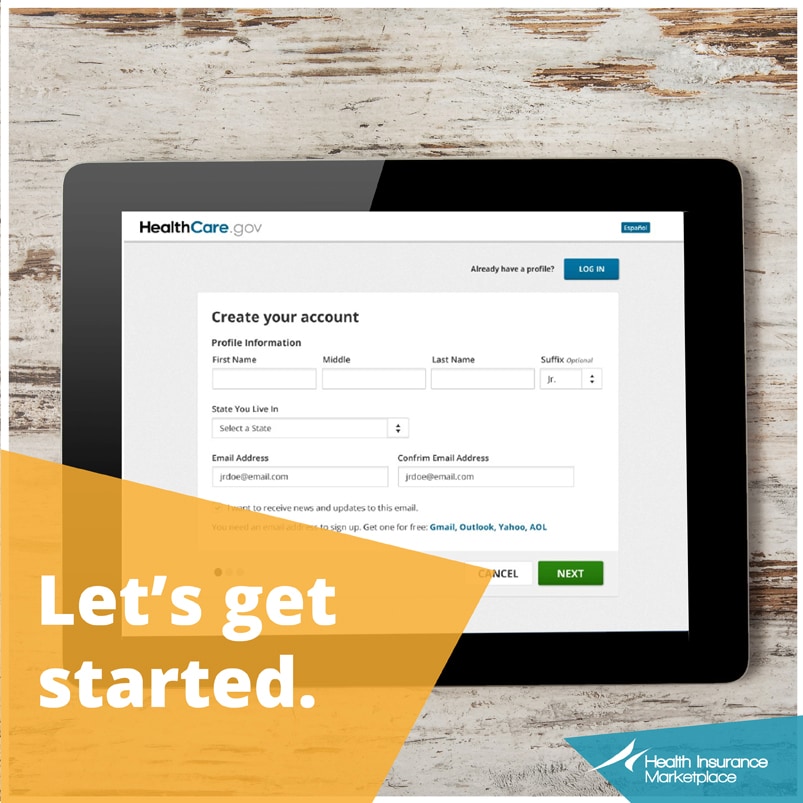
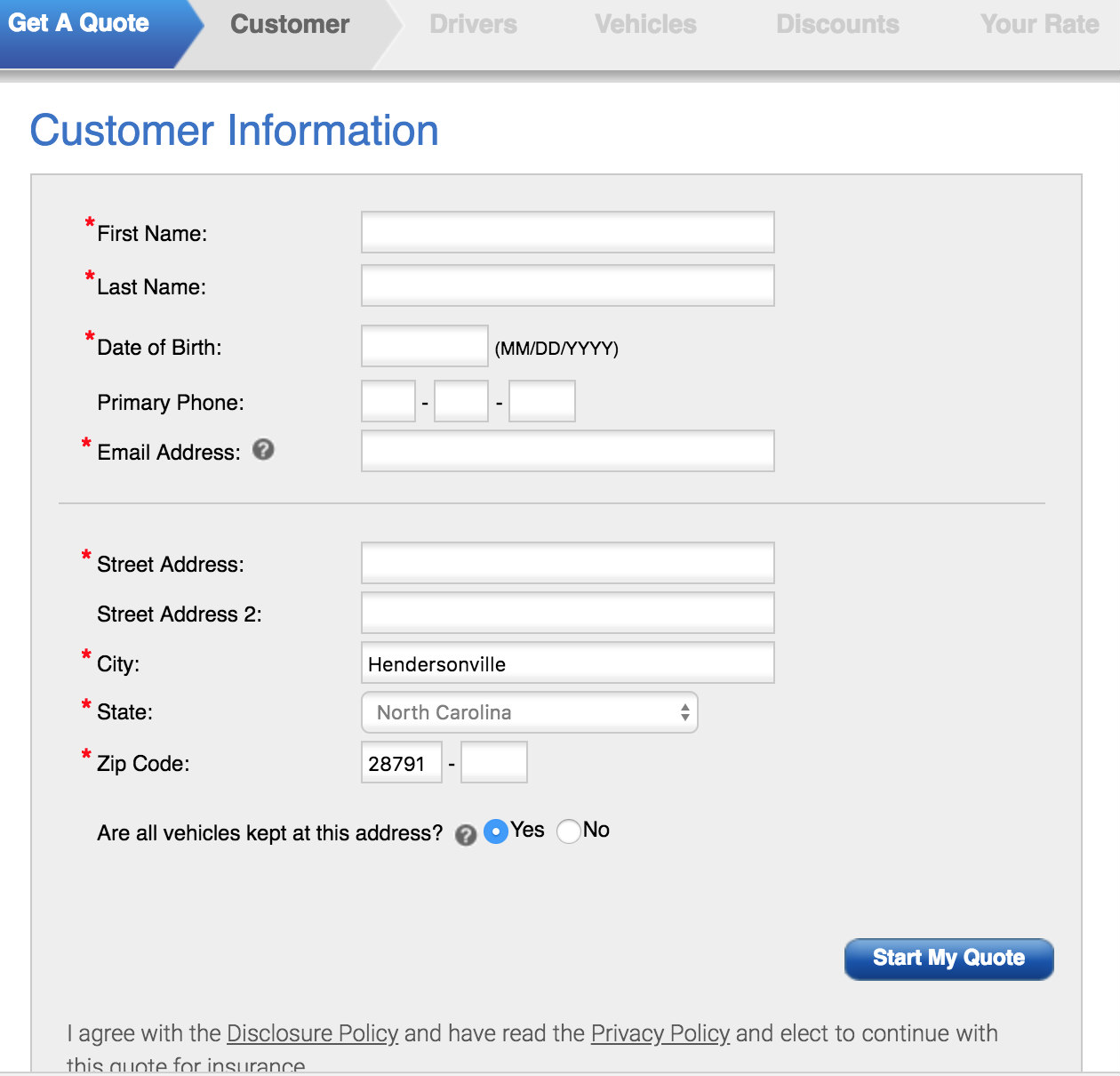
They provide easy-to-use online sales tools to help you get quotes and land sales fast. Accident Fixed-Benefit Brochure Flyer. TrioMED lets you concentrate on your health without worrying about medical bills piling up.
Cutting-edge sales tools and support. Filing a claim is easy and can be completed by logging into your online account. Temporary health care coverage for you and your family.
And it only takes a few minutes. Hospital Expense Protection Brochure. A plan for unexpected out-of-pocket costs associated with accidents critical illnesses and accidental death.
TrioMED is National General Accident and Healths AMECIADD Ancillary product About Press Copyright Contact us Creators Advertise Developers Terms Privacy Policy Safety How YouTube. Auto RV Home Renter Condo Health Commercial Auto. Accident Medical Expense coverage helps you with accident-related health care costs and other expenses.
TrioMED Benefit Maximum 2500 5000 10000 Spouse 50 Dependent Children 25 With three maximum benefits amounts to choose from TrioMED provides the nessary coverage. Eight benefit levels for accident medical expense critical illness and accidental death and dismemberment. Their dedicated team of sales professionals is ready and waiting to help you succeed.
Request a National General Contract today. Eight benefit levels for accident expense cancer and heartstroke and sickness hospitalization. National General Insurance Company Suite of Products.
TRIOMED CANCER and HEARTSTROKE. Cancer HeartStroke Brochure Flyer. TrioMed Brochure Flyer.
TrioMED from National General is a supplemental usually low-cost plan that can be added on to any primary insurance plan including employer plans individual health insurance plans and short-termcatastrophic plans that gives you a cash benefit to help pay unexpected expenses. NATIONAL GENERAL FOUNDATION HEALTH. Dental Indemnity Plan Brochure Flyer.
Five benefit levels available. A plan for out-of-pocket costs associated with accidents critical illnesses and accidental death. TrioMED A plan for unexpected out-of-pocket costs associated with accidents critical illnesses and accidental death National General Accident and Health markets products underwritten and issued by National Health Insurance Company Time Insurance Company Integon National Insurance Company and Integon Indemnity Corporation.
Hier sollte eine Beschreibung angezeigt werden diese Seite lässt dies jedoch nicht zu. Wissenschaftliche und klinische Studien zeigen dass medizinische und chirurigische Bänder die in der Gesunheitsversorgung verwendet werden häufig mit pathogenen Bakterien kontaminiert sind. National General Critical Illness-Term Life.
Get three types of coverage in one plan. Click the button below to continue.




/GettyImages-603707289-57310e865f9b58c34ce03555-c99023fc8b4b4855990ca0ac0a990a82.jpg)