Community-Based Adult Services CBAS and. Contact Anthem HealthKeepers Plus Provider Services to reach staff in any of the following departments.
 Fillable Online Anthem Prior Authorization Form For Procedures Fax Email Print Pdffiller
Fillable Online Anthem Prior Authorization Form For Procedures Fax Email Print Pdffiller
Utilization Management UM for Medi-Cal Managed Care Medi-Cal Phone.
Anthem prior authorization phone number. This includes but is not limited to authorization covered benefits and services and claims submittal. The resources below will direct you to the right place. To ensure a seamless transition.
Recommends submitting prior authorization requests for Anthem HealthKeepers Plus members via Interactive Care Reviewer ICR a secure Utilization Management tool available in Availity. Interpreter services are available over the phone or through telehealth. Select the Drug List Search tab to access up-to-date coverage information in your drug list including details about brands and generics dosagestrength options and information about prior authorization of your drug.
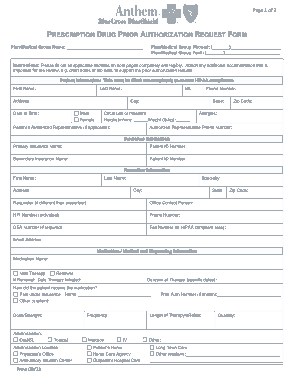
Also specify any allergies and give the name and phone number of the. To request a prior authorization from Utilization Management. Step 1 At the top of the form supply the planmedical group name planmedical group phone number and planmedical group fax number.
Step 2 In Patient Information provide the patients full name phone number full address date of birth sex mf height and weight. If you have questions please contact your group administrator or your Anthem network representative. Effective November 4 2018 please use the below fax number to submit all Anthem pharmacy PA requests for prescription drugs.
800 531-4450 or such other number indicated below for specific services. Phone number on the back of the members ID card or 800-274-7767. Anthem blue cross californiapo box 9051oxnard ca 93031.
57 Zeilen 844-421-5662 Anthem Medicare Individual Business 800-676-2583. Request For Prior Authorization Form - Highmark Blue Cross. In the united states puerto rico and us.
For eligibility-related questions call the number on the back of the members ID card or dial 800-676-BLUE 2583. Please fill out the Prescription Drug Prior Authorization Or Step Therapy Exception Request Form and fax it to 877 327-8009. Fax this form to 1-844-512-7024.
For telephone PA requests or questions please call Provider Services at 1-855-558-1443. While ePA helps streamline the prior authorization process providers can also initiate a new prior authorization request by fax or phone. Phone our Utilization ManagementAuthorization department at 1-888-831-2246 Fax PA requestsquestions to 1-800-754-4708 For Healthy Families Program AIM and MRMIP.
Precertification is required for the following services. The PrecertificationPrior authorization number is listed on the back of the members Anthem ID card. Fax number.
Providers and staff can also contact Anthem for help with prior authorization via the following methods. Anthem Blue Cross and Blue Shield Healthcare Solutions Medicaid Managed Care Pharmacy Prior Authorization Form Page 4 of 4 Billing facility information Name. Anthem Blue Cross Anthem is streamlining its pharmacy intake and prior authorization PA process for its Medi-Cal Managed Care Medi-Cal members.
Creating an account is FREE. Not all PA requirements are listed here. You can also check status of an existing request and auto-authorize more than 40.
Top 10 Anthem Blue Cross Blue Shield Prior Authorization Phone Number Wallpaper. Care Management support is available 247 through Anthem Blue Cross Cal MediConnect Plan Customer Care at 1-855-817-5786. In person interpretation services are available on a case by case basis and must be prior.
ICR offers a fast efficient way to securely submit prior authorization requests with clinical documentation. Health insurance can be complicatedespecially when it comes to prior authorization also referred to as pre-approval pre-authorization and pre-certification. PRIOR AUTHORIZATION CRITERIA IS SUBJECT TO CHANGE.
Weve provided the following resources to help you understand Anthems prior authorization process and obtain authorization for your patients when its required. Prior authorizations are preloaded for the provider before the expansion date. Prior Authorization number for prescription drugs.
Inpatient SurgicalInpatient Medical Admission. Office contact name. Incomplete forms will delay the prior authorization process The completed form may be FAXED TO 1-844-512-7020 for Retail Pharmacy or 1-844-512-7022 for Medical Injectables.





:max_bytes(150000):strip_icc()/medicare-part-d-coverage-4589853-ada67299bb5a4d3eb70e32dd66bcab0f.png)