CVS Caremark administers the prescription benefit plan for the member identified. CoverMyMeds is the fastest and easiest way to review complete and track PA requests.
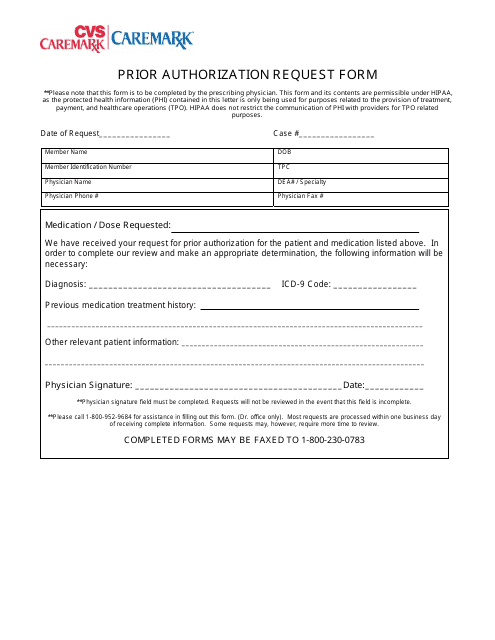 Prior Authorization Request Form Cvs Caremark Download Printable Pdf Templateroller
Prior Authorization Request Form Cvs Caremark Download Printable Pdf Templateroller
This patients benefit plan requires prior authorization for certain medications in order for the drug to be covered.
Cvs caremark medication prior authorization form. Fill in the required fields these are marked in yellow. Available for PC iOS and Android. Please contact CVSCaremark at 1-800-294-5979 with questions regarding the prior authorization process.
If the person making the request is representing the enrollee complete the second section as well Step 2 Write the name of the prescription drug you are requesting at the top of page. At CVS Specialty our goal is to help streamline the onboarding process to get patients the medication they need as quickly as possible. Drug Name select from list of drugs shown Lazanda fentanyl citrate nasal spray.
1-866-249-6155 CVSCaremark administers theprescription benefit plan for the patient identified. Forms are being updated and will be made available soon. Download Enrollment Forms.
MASSACHUSETTS STANDARD FORM FOR MEDICATION PRIOR AUTHORIZATION REQUESTS Some plans might not accept this form for Medicare or Medicaid requests. Start a free trial now to save yourself time and money. The CVS Caremark Prior Authorization Request Form can be used to request coverage for a non-formulary medication or one which is more expensive than those which are typically covered by the insurance company.
The below form must be completed in its entirety by the medical practitioner prescribing the drug. Prior Authorization Request Send completed form to. Please contact CVSCaremark at 1-800-294-5979 with questions regarding the prior authorization process.
Prior Authorization can ensure proper patient selection dosage drug administration and duration of selected drugs. Our electronic prior authorization ePA solution is HIPAA-compliant and available for all plans and all medications at no cost to providers and their staff. Prior Authorization Request Send completed form to.
Ormulary ExceptionPrior Authorization Request Form Patient Information Prescriber Information Patient Name. CVS Caremark Prior Authorization PA tools are developed to ensure safe effective and appropriate use of selected drugs. Pharmacists may also initiate a prior authorization after which CVS Caremark will contact the appropriate physicians office to complete the request.
Step 1 The first section of the SilverScript prior authorization form Enrollees Information requires that you provide your name date of birth physical address phone number and member ID. The CVSCaremark prior authorization form is to be used by a medical office when requesting coverage for a CVSCaremark plan members prescription. Select the Get form button to open the document and begin editing.
Fax signed forms to CVSCaremark at 1-888-836-0730. Fax signed forms to CVSCaremark at 1-888-487-9257. This patients benefit plan requires prior authorization for certain medications in order for the drug to be covered.
Case Review Unit CVS Caremark Prior Authorization Fax. CVS Caremarks Preferred Method for Prior Authorization Requests. Case Review Unit CVS Caremark Specialty Programs Fax.
Cvs Caremark Prior Auth Form. This patients benefitplan requires prior authorization for certain medications in order for the drug to be covered. Initial Request ContinuationRenewal Request Reason for request check all that apply.
Physicians may also complete a prior authorization fax form and fax it to CVS Caremark. 1-855-330-1720 CVS Caremark administers the prescription benefit plan for the patient identified. Case Review Unit CVS Caremark Prior Authorization Fax.
Prior Authorization Step Therapy Formulary Exception. A physician will need to fill in the form with the patients medical information and submit it to CVSCaremark for assessment. When conditions are met we will authorize the coverage of Preferred Product Program Exceptions UMWA.
We offer access to specialty medications and infusion therapies centralized intake and benefits. CVSCaremark Prior Authorization Form California Created Date. Complete Cvs Caremark Prior Authorization Form in just several minutes by following the recommendations below.
The most secure digital platform to get legally binding electronically signed documents in just a few seconds. When conditions are met we will authorize the coverage of Lazanda. This form is being used for.
Completereview information sign and date. Prior Authorization Request. CVS Caremark Prior Authorization Fax Forms.
Fill out securely sign print or email your cvs prior form instantly with SignNow. Contains references to brand-name prescription drugs that are trademarks or registered trademarks of pharmaceutical manufacturers not affiliated with CVS Caremark. Find the document template you need from the collection of legal form samples.
Send your specialty Rx and enrollment form to us electronically or by phone or fax. Send completed form to.








/shutterstock_161758760-5bfc47aa46e0fb0026623118.jpg)
