Among the factors that affect your monthly premium rates is the pricing method that your carrier uses. Medicare Supplement Plan N coverage is one of 10 federally standardized options to help fill gaps in original Medicare coverage.
 Transamerica Medicare Supplement Plans For Baby Boomers
Transamerica Medicare Supplement Plans For Baby Boomers
In addition some insurance companies are preparing for Medicare Supplement Plan D to be one of the top selling plans in Medicare.
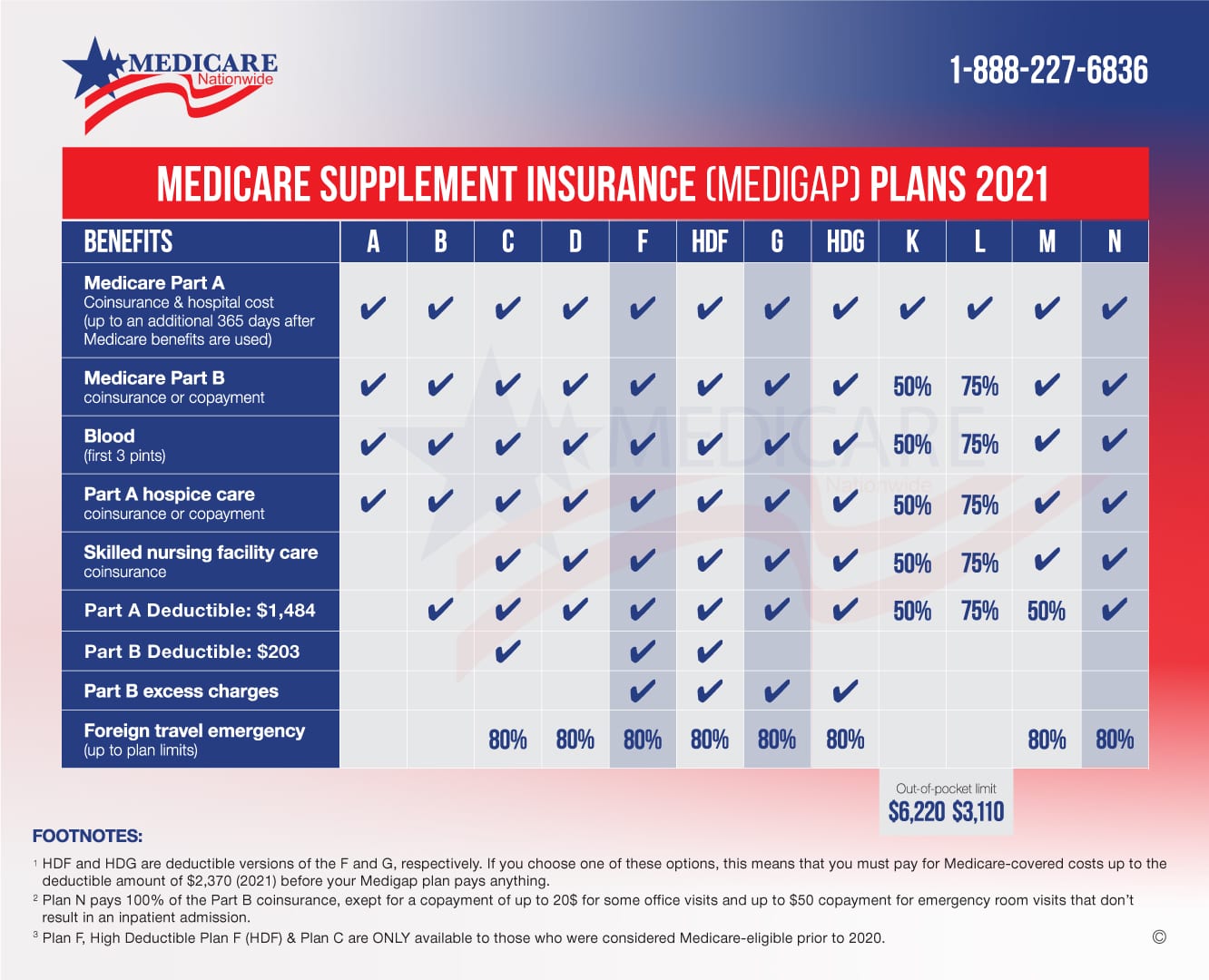
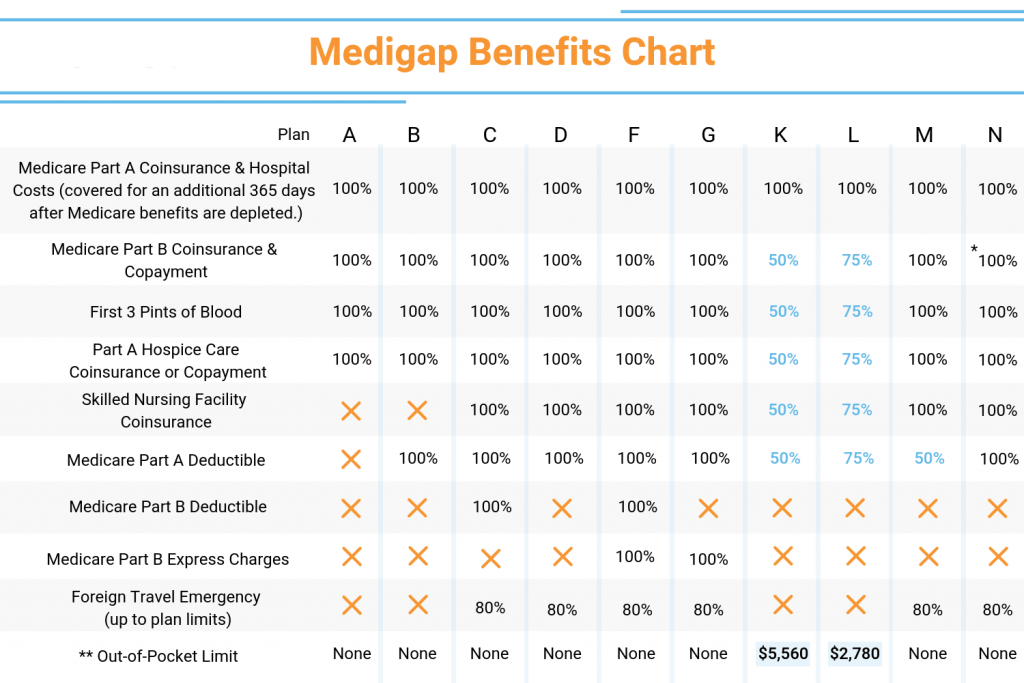
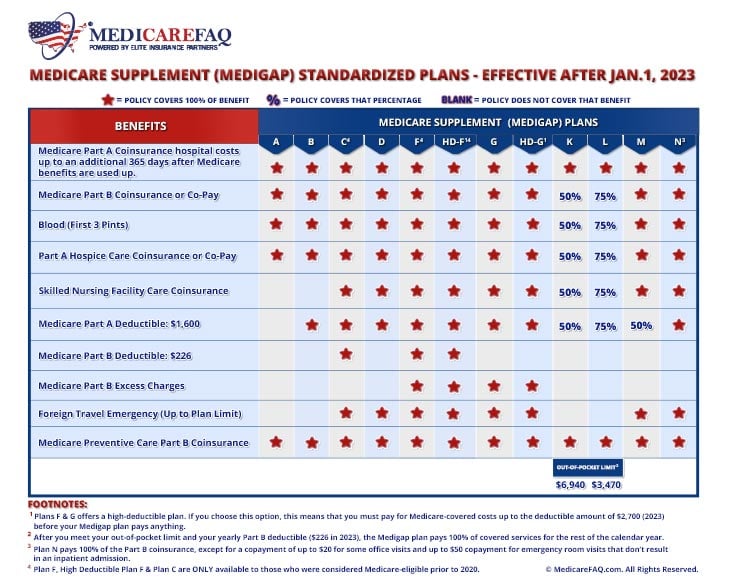
Medicare supplement plan n vs g. 10 rows Medicare supplement plan N is one of the ten standardized plans of Medigap. As mentioned above you can incur Part B excess charges when your health care provider does not accept Medicare assignment. Plan C is a distant second at about 9 according to the most recent Medigap enrollment data.
Contents Of This Video 000 Plan G vs Plan N204 What they cover306 Excess Charges Explained508 Coverage Differences546 Price Differ. Plan N offers the same coverage as Plan G in that it also does not cover the Medicare Part B deductible like Plan F does. In particular Plan G covers excess charges that go beyond Medicares.
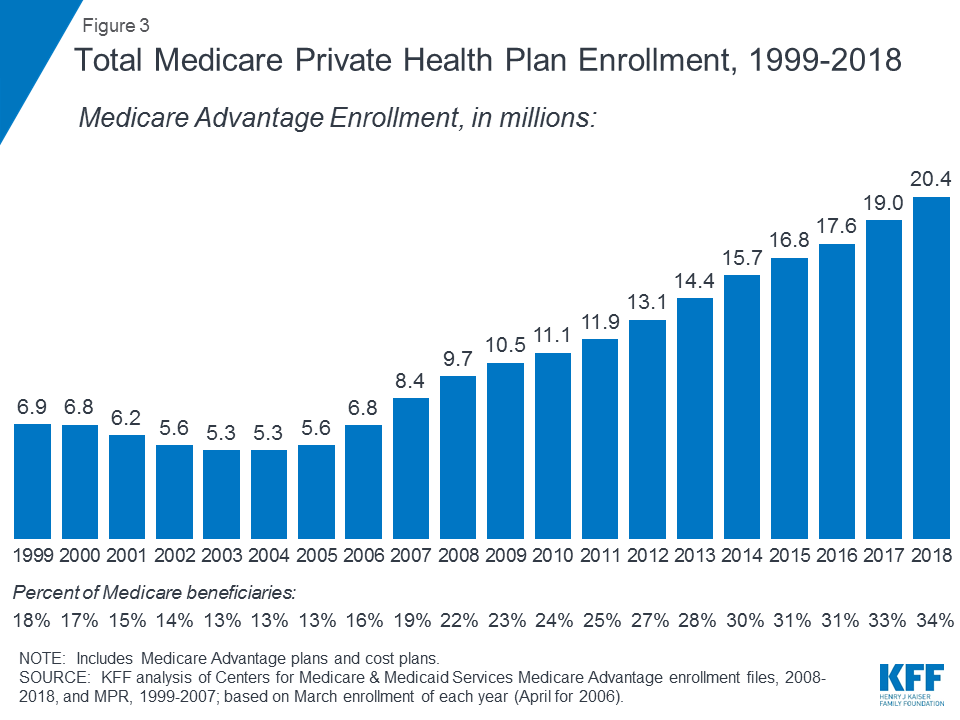
If youre looking for the plan with the highest enrollment growth however Plan N and Plan G are skyrocketing in popularity up 33 and 25 respectively over last years numbers. Diagnostics Equipment Consumables Stethoscopes First Aid Much More. Medigap Plan G Premiums vs.
How Are Plan G and Plan N Similar. It is also one. Depending upon the condition of your health it might be a better idea to sign up for Plan N even though there is a copay and may be 15 in excess charges associated with it.
Medicare Supplement Plan N Rate Increase History. Ad No Account Needed to Order Checkout As Guest For Faster Order Processing. Ad No Account Needed to Order Checkout As Guest For Faster Order Processing.
Its Plan F by a landslideabout 55 of all Medigap plans currently in force are Plan F. Medicare Plan G offers slightly more comprehensive coverage than Plan N but with higher monthly premiums. Its an option for people who want broad coverage but to.
Medicare supplement Plan N can be a better value than Medicare supplement Plan G. This is especially true in states that have specific laws reducing the value of Medicare supplement Plan G. A head-to-head comparison of the Medicare MSA Plan vs Medigap Plan G two of the most popular ways to supplement your Medicare coverage.
Diagnostics Equipment Consumables Stethoscopes First Aid Much More. However it differs from Plan G by not covering Medicare Part B excess charges. These increases are lower when compared to Plan F and.
Medicare Supplement Plan G and Plan N are two of the most popular Medicare Supplement or Medigap plans. In the last five years premium rates for Plan N have increased between 2 and 4. Plan G is the most comprehensive of the two plans but Plan N offers a very good value for a lower monthly premium.
In most states Plan G generally runs about 20-25 more per month than Plan N More about Plan G prices. Today were going to highlight the benefits of Medicare Supplement Plan G vs N. Medigap Plan N Premiums.

















:max_bytes(150000):strip_icc()/medicare-part-d-coverage-4589853-ada67299bb5a4d3eb70e32dd66bcab0f.png)






