Medications subject to change without notice. But if you have surpassed your annual limit or you havent yet met your deductible for the year or for the incident which is how some policies work you may not be covered at all.
 Fluticasone Propionate Nasal Spray Dosage Instructions Ppt Download
Fluticasone Propionate Nasal Spray Dosage Instructions Ppt Download
Aerobid-M Covered Formulary AlternativesAzmacort Flovent Flovent Rotadisk Pulmicort Turbuhaler.
Flovent not covered by insurance. I dont have that kind of money on Social Security. Where differences are noted between this list and. Be injected infused or taken by mouth.
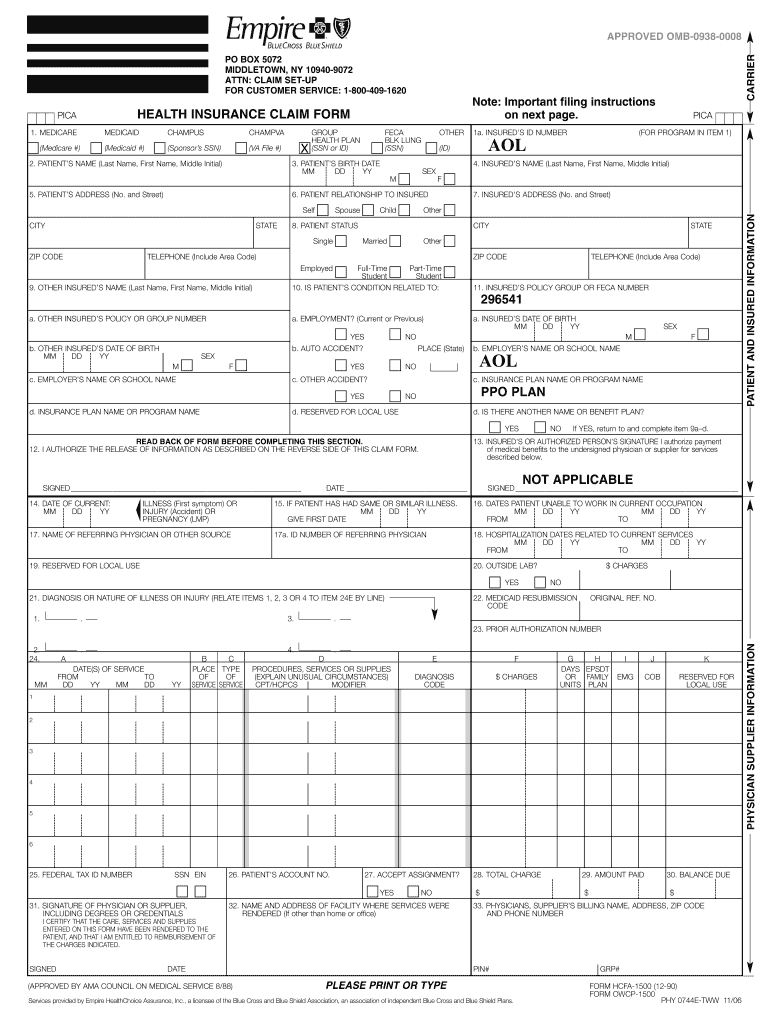
I am getting over the flu and my doctor prescribed a Flovent inhaler for my asthma. The process of getting the insurance company to pay its share of the bill is usually quite straightforward. Open the cover of the inhaler until you hear a clicking sound.
Pricing and Coupons Prices are without insurance. Covered Formulary AlternativesNiaspan lovastatin generic for Mevacor Non-Formulary Drug. The counter counts down by 1 each time you open the cover.
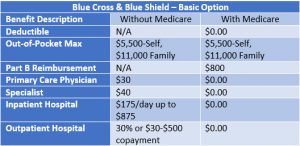
Blue Care Network reviews all physician and member requests to determine if the drug is medically necessary and if there are equally effective alternative drugs on the formulary. Flovent is a liquid form of fluticasone used with an inhaler device. An albuterol inhaler can run those who suffer from asthma between 30 and 80 without insurance depending on whether its a brand name or generic version and whether you have a.
Show them the list of preferred alternatives. Below is a list of medications that will not be covered without a prior authorization for medical necessity. Before you use this medicine the counter should show the number 30.
Review your benefit plan documents to see what medications are covered under your plan. Aerobid Covered Formulary AlternativesAzmacort Flovent Flovent Rotadisk Pulmicort Turbuhaler. Flovent Diskus ArmonAir and Arnuity Ellipta are powder forms of fluticasone that come with a special inhaler device preloaded with blister packs containing measured doses of fluticasone.
Medications used to treat cold or cough symptoms. Thats because many health plans have a lower co-payment for generics. You and your doctor can decide.
Are not used for a medically accepted purpose. The device opens and loads a blister of fluticasone each time you use. And even if patients do not have to pay the full price they may still save money.
Lower-cost options are available and covered. Not all medications listed may be covered under your benefit plan. Refer to plan documents.
Some examples of medications that may not be covered by Medicare include. We could not find an exact match for this medicine. This is not a complete list of medications and not all medications listed may be covered under your plan.
This device creates a spray that you inhale through your mouth and into your lungs. Coverage may not apply in all plans. Weight loss or weight gain medications.
I cant afford one not to mention a maintenance RX for 3 months. In most cases if you fill a. Both medications are similar to Advair Symbicort Dulera and Breo.
Are not approved by the Food and Drug Administration. The drugs shown below arent covered on the commercial Blue Cross Blue Shield of Michigan PPO and Blue Care Network HMO drug lists. This is more likely to work in cases where youve tried the other options and they dont work for you or theres a medical reason why you arent able to take the covered alternative.
See the full Flovent side effects document. Are sold or used outside of the United States. Try searching the Price Guide directly.
Our specialty pharmacy can provide most of your specialty medications along with helpful programs and services. Finally get in touch with your doctor and explain that your current prescription will no longer be covered by your insurance in 2015. The inhaler is now ready to use.
If you open and close the cover without inhaling the dose you will lose the medicine. If you got the medication from a local or online pharmacy simply provide the insurance company with a copy of the. We will notify both you and your doctor in writing if the request is.
Its not unusual for me to use my short-acting inhaler several times a day but my insurance will only cover one Proventil inhaler every 60 days. One inhaler would cost me 30000 I used to get these for a simple copay. In comparison this new generic inhaler costs between 50 and 90.
A drug thats not in our formulary sometimes called a drug list may require prior authorization. My insurance doesnt cover ANY steroid inhalers Secure HorizonsUnited Healthcare for seniors. I feel like Im sacrificing my health trying.
See the full Symbicort side effects document. Those typically cost between 300 and 400 per prescription. If you continue using one of these drugs without prior approval you may be required to pay the full.
Call 1-855-427-4682 and have your prescriptions delivered right to your home or. Do not close the cover until you have taken your dose. See the full Advair Diskus side effects document.
Or it might not be a covered benefit under your drug plan. Please note not all specialty medications are listed in the formulary.