The answer depends on whether or not the reduction is deemed medically necessary as well as the terms of the health insurance coverage. The insurance companies want to see that you are having symptoms due to the size of your breasts.
 How To Get Breast Reduction Surgery Covered By Your Insurance Aesthetica Blog
How To Get Breast Reduction Surgery Covered By Your Insurance Aesthetica Blog
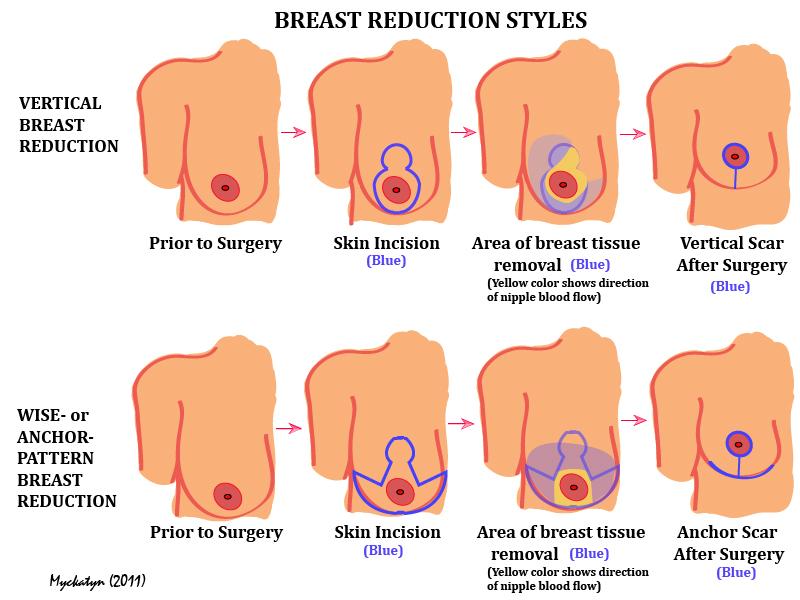
Breast reduction surgery is done to change the size weight firmness and shape of the breasts.
Will insurance pay for breast reduction. Will insurance pay for a breast reduction. Hence the patient needs to show valid medical reasons for opting for breast reduction surgery. Find a facility or a few that you are interested in where you may consider having the surgery.
There is such a thing as medically necessary breast reduction. Rarely will an insurance company pay for a cosmetic procedure. A plastic surgeon who performs breast reduction surgery on a regular basis will work diligently with you to get your insurance company to cover the procedure.
This means that your carrier will not cover breast reductions no matter the reason even if your doctor says it is medically necessary. 1 Insurance companies try very hard not to pay for breast reduction even though they should. Not too long ago breast reduction surgery was not covered by insurance at all.
You may decide to have breast reduction surgery to. Youll need to get your breast. Unfortunately large breasts alone without symptoms are not enough.
2 Very big reductions like from an. There are many cases where health insurance covers some or all of the costs of a breast reduction. The important distinction is which reduction.
The payments made to the chiropractor. On the subject of whether or not your health insurance provider will cover your breast reduction procedure this will differ depending on the health insurance company and their breast reduction requirements. Even small breast reductions relieve many symptoms such as back pain and shoulder pain and even some types of headaches.
While these are not medical proof you need back pain it gives insurance company a better idea of why you should have breast reduction surgery insurance covered. Although the process of getting breast reduction surgery covered by insurance can be challenging it can save you a considerable amount of money provided your claim is approved. Health Insurance May Cover Breast Reduction.
According to data compiled by the American Society of Plastic Surgeons the average cost of a breast reduction surgery is 5482 which includes the following additional fees. They want to see that these symptoms do not improve with other treatments. Unless you can privately pay for your breast reduction surgery it is recommended to do the following before your breast reduction procedure to see about insurance coverage.
It required an act of Congress for having large heavy breasts to be acknowledged as a cause of multiple medical conditions including. However as a general rule breast reduction is typically considered a cosmetic procedure. Spinal curvature with back and shoulder problems rashes a reduced ability to exercise due to the physical weight as well as psychosocial shame.
Some insurance companies wont cover breast reduction unless the surgeon plans to remove at least 500 grams more than one pound of breast tissue on both sides even though studies have shown that the amount of tissue removed is unrelated to relief of symptoms. However patients must meet a number of criteria before their insurance will pay for this surgery. Check your insurance policy to see if such a procedure could be covered or partially.
Breast reduction surgery can eliminate. A breast reduction surgery can have many great benefits and help you live a more confident active lifestyle. It is also important to note that the combination of a high deductible and copayment requirements sometimes make it less expensive to pay outside of your insurance.
As long as your insurance. If you have medical issues that require breast reduction to remedy the problem most insurance companies will pay for the procedure. Breast Reduction Coverage Blue Cross Blue Shield In some cases insurance will pay for part or all of a womans breast reduction surgery.
Do not throw away receipts from your chiropractor More often than not the excess weight in the breast region causes a lot of stress on the back and the neck region. Breast reduction is one of the most popular procedures that plastic surgeons do and typically breast reduction patients are very happy with their results. As a result most women visit a licensed chiropractor to seek relief from pain caused by this stress.
Some of these can include upper back shoulder and neck pain rashes under the breasts and grooves on the shoulders due to your bra straps. With that said health insurance typically does not cover cosmetic plastic surgery except to restore the body to proper function after an injury to repair certain function-impairing birth defects and for reconstruction of one or both breasts after a mastectomy. Medicare will pay for breast reduction in the case of hypertrophy as long as your doctor states that it is the primary cause of your pain or other symptoms.
This typically depends on whether or not your insurance company regards the procedure as medically necessary. It is one of the few plastic surgery procedures that is covered by insurance. Large heavy breasts can cause back and neck pain skin irritation and posture problems.
Speak to a surgeon who you want to perform the breast reduction. The constant pull of heavy breasts may make bra straps leave painful indentations in your shoulders. Breast reductions can be covered under insurance if certain criteria have been met.