Providing an identification card ensures the safety of the parties involved. If you need to pick up a medication you should absolutely do so but you will have to pay the full price for the medication up front as your ID card is not available yet.
Cvs Caremark To Be Prescription Benefits Manager For Nyc Transit On June 1 Twu Local 100
If you need to fill a prescription you can obtain your BCBS ID information on the student insurance portal.
Prescription id card. Many translated example sentences containing prescription id card Spanish-English dictionary and search engine for Spanish translations. Learn how to find your BCBSMA member ID. The card only has a code number the name of the hospital and an authorized signature.
How much does this card cost. Now as always were here to help. You can also access CIGNAs website to request a replacement ID card or an additional ID card for any covered participant.
PrescriptionCards formerly AxiaRx is the only prescription discount card that provides a donation to local charitable animal welfare organizations like humane societies and SPCAs. Card issuer name or logo. When ordering or picking up your prescriptions please provide the infomation on this Zion Prescription card along with your member number listed on your Zion Health ID card.
Prescription Drug ID Card. ZION HEALTHO OPTUMRx Payer Id. At a participating retail pharmacy by providing your new CVS Caremark prescription ID card to the pharmacist.
The name or logo of the benefit administrator issuing the identification card. To check medical records submit tax claims etc. Safe accurate prescriptions delivered to your door.
The visitor identification card is quite different among other medical ID cards. 1 Pharmacies will reimburse you for a prescription if you come back with your insurance information at a later date. Call the myMatrixx an Express Scripts.
Thanks to the ID-card Estonia has one of the worlds most advanced digital signature systems. Questions or need assistance locating a participating retail network pharmacy. Many prescription cards offer regular coupons or discounts on prescriptions or act as a type of rewards card where the customer earns points towards a discount with every prescription purchased.
To learn more about the ID-card visit its webpage. A prescription card is a card issued by a pharmacy to a customer to keep track of the prescriptions purchased. A Pharmacy Benefit Program handbook and a long-tem card will be sent to you once compen-sability has been determined.
Express Scripts is the countrys largest pharmacy benefit manager and one of the largest pharmacies. Each time the partners prescription discount card is used our humanecard program donates 51743 since 2012 to 32 charities from New York to California. United Health Care - A UnitedHealth Group Company.
Finding a participating pharmacy is easy nine out of 10 pharmacies nationwide. Front of Pharmacy-only ID Card Requirements. Your Blue Cross Blue Shield BCBS ID number is also used to fill prescriptions.
The card is issued at no cost and covers approved work-related injury prescriptions. Search compare prescriptions drug prices and save at over 60000 pharmacies and Amazon Pharmacy. A prescription card may also keep track of other non-prescription.
65241 Mailing Address PO Box 21747 EaganMN 555121 Member Care 888-920-9466. Pharmacy listed on the back side to speed the processing of your approved workers compensation prescriptions. The back of the member ID card may include phone numbers to connect with customer service speak with a nurse and find behavioral health support.
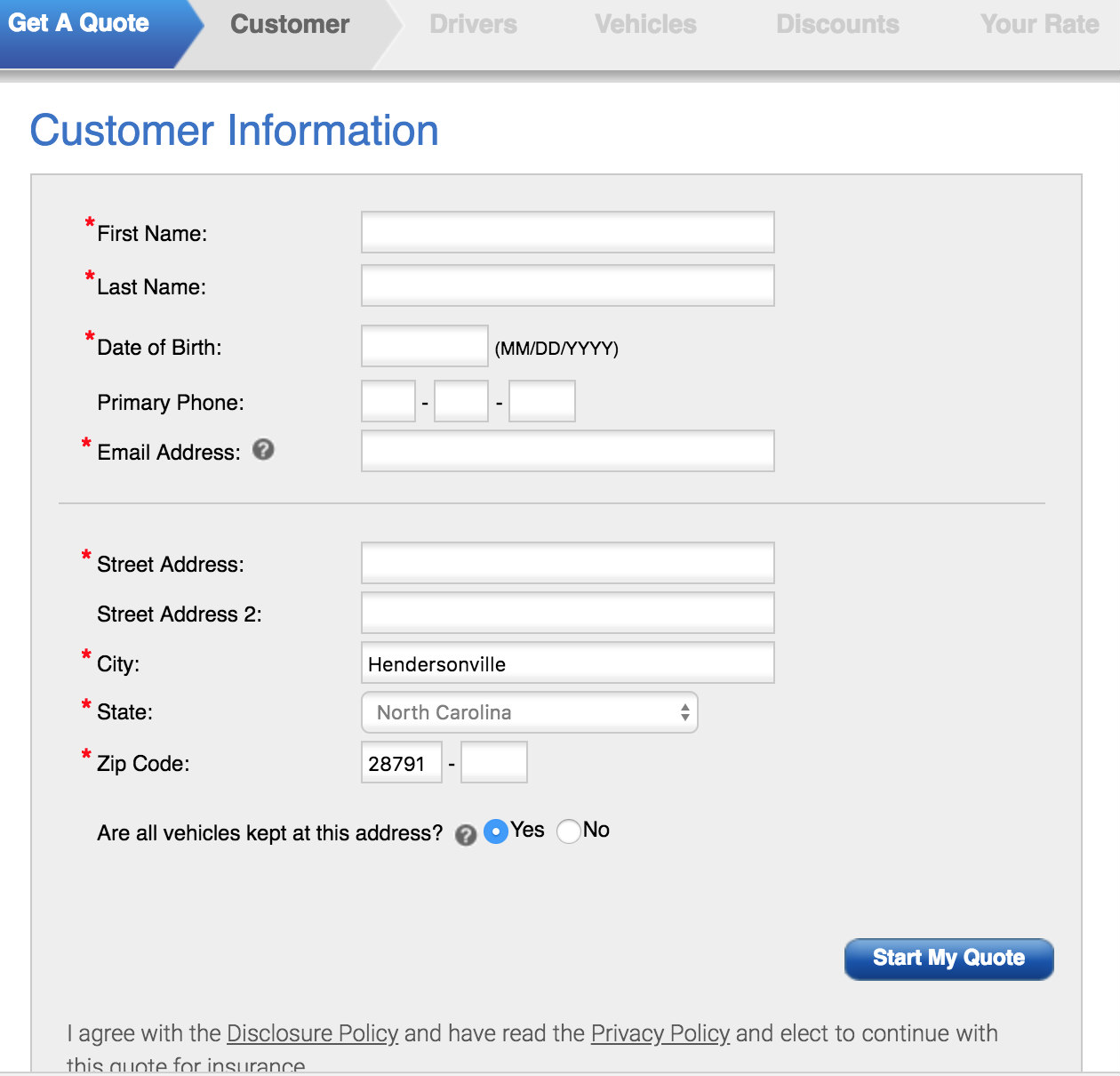
Outsiders visiting the hospital can sometimes be a risk for some patients visitors and employees. When your plan includes pharmacy benefits your pharmacy will need to verify your coverage when filling prescriptions. This information is to be located at the top of the card.
Workers Compensation Temporary Prescription ID Card To the Injured Worker. However there are options to get reimbursed quickly. Prescription ID Card until you receive a permanent card.
Save on Prescriptions with Prime with your Amazon Prime Prescriptions savings card. The program offers an average savings of 20 percent off the regular retail price. ID cards showing your new member PICA ID number to use your prescription drug plan.
They vary in how long they give you to come back but many will. On your first visit please give this notice to any. Pharmacy-only ID cards are used solely to provide information about pharmacy benefits.
Can I use the Temporary Prescription ID Card right away. Present the prescription ID drug Card along with your prescriptions ate a participating pharmacy. National health insurance card.
When you choose to go to a non-participating pharmacy you will pay the full cost of the medication. These cards with your new PICA ID number replace any previous PICA Express Scripts member ID cards you may have and should be used by all covered family members. If you use a non-participating pharmacy you should submit a paper.
Proof of identification when logging into bank accounts. Please give this card to your pharmacy the next time you have a prescription filled for an injectable or chemotherapy medication. Moreover providing an ID card to visitors makes them aware of the.
World-class customer support 24x7.