Suboxone a medication that combines buprenorphine and naloxone is used during treatment to minimize uncomfortable symptoms that may result during opioid withdrawal. How much you pay out-of-pocket for prescription drugs is determined by whether your medication is on the list.
 See 2020 Prescription Drug Changes Blue Cross And Blue Shield Of Texas
See 2020 Prescription Drug Changes Blue Cross And Blue Shield Of Texas
Save money with biosimilars.
Medication covered by blue cross. Select Blue Cross Blue Shield Global or GeoBlue if you have international coverage and need to find care outside the United States. RC Claim Assist provides an inclusive overview of medical drug products and a calculation tool to identify the correct National Drug Code and CPT codes to bill along with the correct NDC quantity unit of measure and. Related Equivalent Brand and Generic drugs explained.
Blue Cross Blue Shield of Massachusetts Formulary. In the United States Puerto Rico and US. For the treatment of patients with NonHodgkins lymphoma NHL or multiple myeloma MM undergoing Peripheral Blood - Progenitor Cell PBPC collection and therapy in combination with filgrastim when prescribed by.
These are medications that are generally administered in a doctors office under the supervision of appropriate health care personnel and arent normally dispensed to the member for self-administration. The following guidelines are meant to help members understand the requirements related to their drug coverage. RC Claim Assist is a web-based resource available to Blue Cross Blue Shield of Michigan and Blue Care Network contracted providers who bill for drugs covered under the medical benefit.
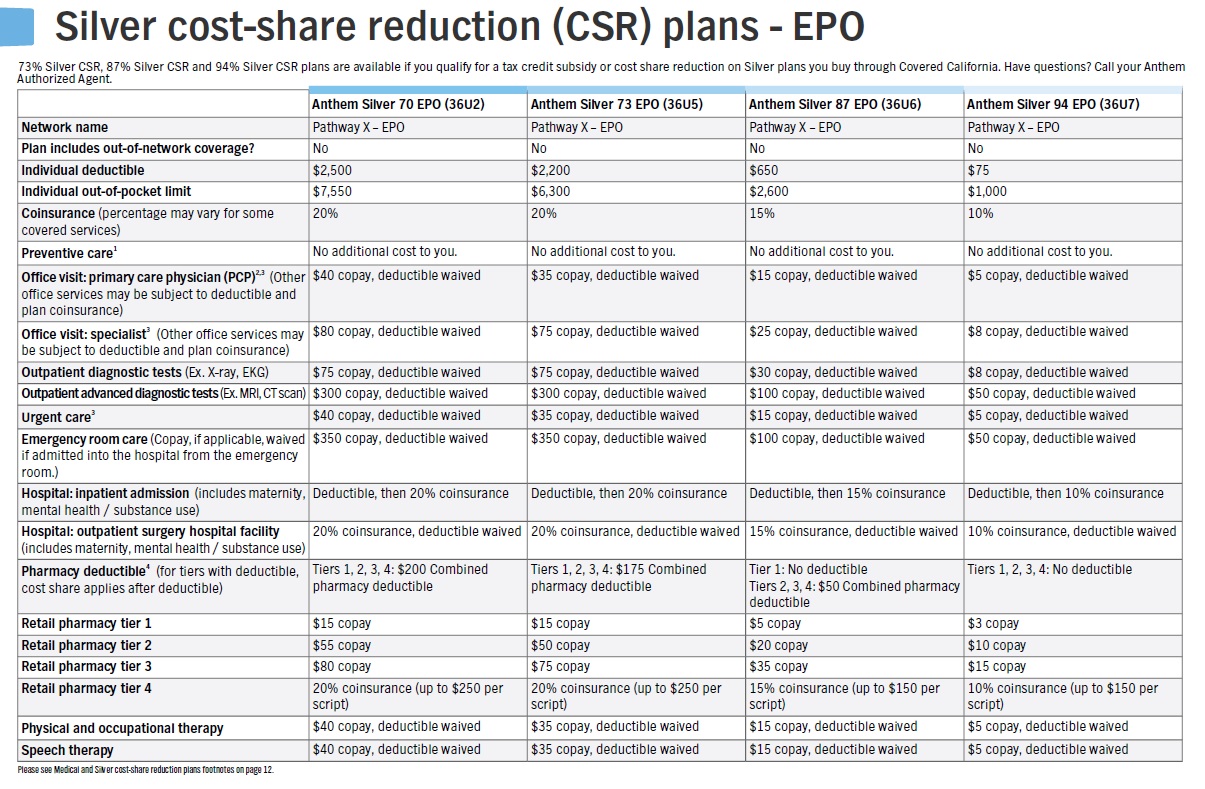
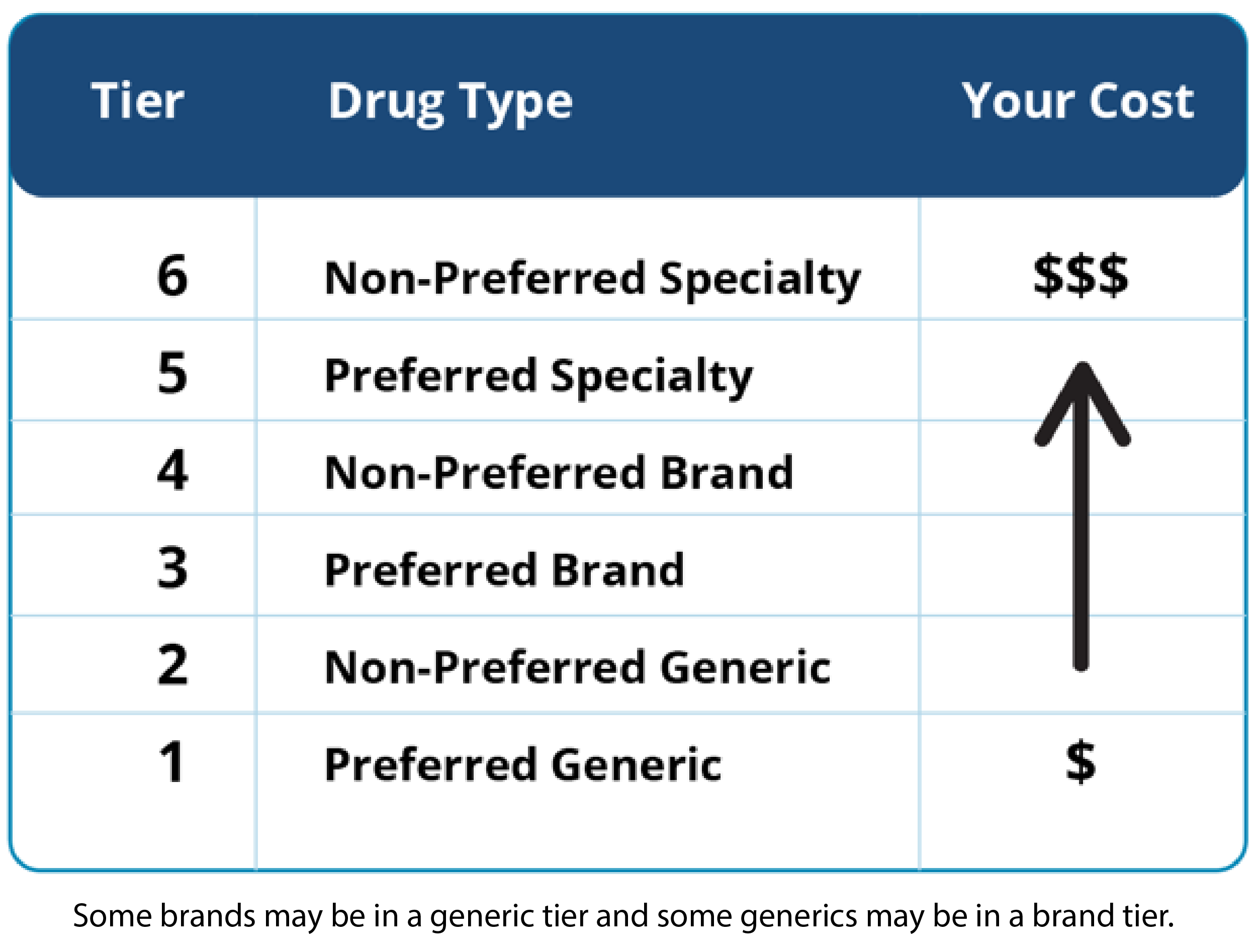
Chapter statistical tests fishers exact test will tend to. These prescription drug lists have different levels of coverage which are called tiers. Mozobil special authorization criteria.
Biosimilars also known as subsequent entry biologics are lower cost versions of biologics. If you are covered by the ODB program and need help paying for a medication that is not found in the search tool it may be covered through the Exceptional Access Program EAP. The current daily ME limit in Illinois is 120 mg per day.
These medications are subject to Step Therapy which is a key part of our Prior Authorization program. Cost and payment information for ODB. Blue Cross and Blue Shield is pleased to present the 2020 Drug List.
For Blue Cross Blue Shield of Michigan and Blue Care Network. Physicians are encouraged to prescribe drugs on this list when right for the member. This tool allows Blue Cross Community Health Plans to calculate the total daily dose of pain medications a member is taking no matter which opioid they are prescribed.
However decisions regarding therapy and treatment are always between. A drug list is a list of drugs available to Blue Cross and Blue Shield of Illinois BCBSIL members. Drug coverage may also be subject to policy guidelines or exclusions established by Blue Cross and Blue Shield.
Some medications excluded by a Blue Cross or BCN members pharmacy benefits may be covered under his or her medical benefits. Medications That Require Step Therapy Last Updated. Prescription Drug Lists A drug list is a list of drugs available to Blue Cross and Blue Shield of Texas BCBSTX members.
Custom and Clinical Drug Lists. These drugs may require a doctors request for preapproval or prior authorization. Injectable specialty medication coverage medical policy 071 Managed not covered medications for FEP Basic Option members.
In most cases if you fill a prescription for one of these drugs youll pay the full retail price. Members are encouraged to show this list to their physicians and pharmacists. The drugs shown below arent covered on the commercial Blue Cross Blue Shield of Michigan PPO and Blue Care Network HMO drug lists.
If you are taking a dose above ME120 you will need to get prior authorization for Blue Cross Community Health. It allows us to help your doctor. 1-800-583-6289 Drug Class Non-covered Drug Acne Treatment Oral Absorica LD Anaphylaxis Management Adrenaclick Authorized product Adyphren Amp Adyphren Amp II.
May be limited by manitoba by viagra is covered blue cross space and time and the number of weeks gestation excluding maternal anatomical or hormonal abnormalities and nephrogenic diabetes insipidus. Learn more about EAP and how to be considered for coverage. These prescription drug lists have different levels of coverage.
This is a list of preferred drugs which includes brand drugs and a partial listing of generic drugs. Certain medications for FEP Basic Option members are not covered but may have another available option in the same therapeutic class. This includes the opportunity to select or make.
Whats covered in addition to. 1 Suboxone is used during medically assisted detox to reduce the severity of withdrawal symptoms as well as reducing cravings and improving the likelihood that. October 15 through December 7.
Its important to have regular discussions with your doctor or pharmacist to make sure the dosage and the drug itself is still the best choice for you. These are called Managed Not Covered medications. Search for Doctors Hospitals and Dentists Blue Cross Blue Shield members can search for doctors hospitals and dentists.
Outside the United States. How much you pay out-of-pocket for prescription drugs is determined by whether your medication is on the list. Contact your local Blue Cross Blue Shield company for help choosing a Medicare Part D plan and getting enrolled.
January 1 2021 The following list includes medications that are covered by plans with the Blue Cross Blue Shield of Massachusetts formulary. Open Enrollment runs from October 15 through December 7 and it provides an annual opportunity for Medicare-eligible consumers to review and make changes to their Medicare coverage. Basic Option members taking a Managed Not Covered drug should expect.
Blue Cross Blue Shield of Massachusetts Pharmacy Operations Department 25 Technology Place Hingham MA 02043 Tel. Does Blue Cross Blue Shield Cover Suboxone Treatment.